Latest Resources

Will Changes to Contracts and Funding Really Make the NHS Fairer?
As the government promises to align NHS funding more closely with health need, contracts and payment rules are moving to the centre of the inequalities debate. In the second blog of our three-part series, we examine whether the 10 Year Health Plan’s proposed funding reforms — from revisiting the Carr-Hill formula to introducing capitation and new neighbourhood contracts — can meaningfully redirect resources towards the communities that need them most.

Health inequity is built into policy, not into people
Health inequity is not the product of individual behaviour, but of policy design. Drawing on a comprehensive synthesis of recent evidence, this blog examines why public policies that reshape social and material conditions are more likely to reduce health inequities than those that rely heavily on individual agency, and how a policy-focused framework can help anticipate these effects.
Displaying 37-45 of 69 results.

“The more we know about ourselves the more we can grow as a people”
In this blog, Sharon Cumberbatch, an NHS nurse, shares her life story as a first-generation black British Caribbean, a health care trainee and a health care professional. In honour of Black History Month, Sharon reflects on the aspirations that have driven her in life, her experiences of systemic racism but also experiences of solidarity. She highlights the importance of learning – about the world but also about our own and others’ histories – as the cornerstone of caring communities.
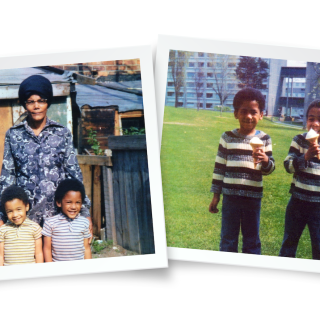
Ripple Effects: Reclaiming Our Stories
In this blog, Chris Frederick, a Lived Experience Advisor, explores how his life has been shaped by the intergenerational and historical trauma experienced by his family and within black communities. In honour of Black History Month, Chris traces the connections between the Windrush Generation, the Brixton riots, and the rise of Black mental health advocacy in the 21st century, highlighting the ongoing work of black communities to address health inequalities and tackle mental health stigma.

Harnessing Health Impact Assessments for a fairer and healthier future
A healthy population is key to citizen wellbeing, a productive economy and manageable public services. Policy decisions on jobs, income, housing, education, transport and green space have a major impact on health, but do not involve the Department of Health and Social Care. As the government sets out policies to deliver on its manifesto commitments, how can we ensure health is considered across government, mitigating the potential adverse impacts, ensuring equity and accentuating the positives? Here we argue that Health Impact Assessments are a key tool to cross-government action on health and health inequalities.

Making Health in All Policies a reality: A call for Health Impact Assessments across government to improve health and address health inequalities
In this evidence brief, we examine the current state of Health Impact Assessments (HIAs) in the UK and their potential to reduce health inequalities. HIAs are essential to the Health in All Policies approach, which integrates health considerations across government. We offer recommendations to increase HIA use, emphasising the need for stronger leadership and dedicated resources to fully embed HIAs in national policy-making.

Feeding two birds with one scone: Leveraging NHS anchor activity to reduce health inequalities and contribute to thriving communities
Discussions around population health and economic growth and their interconnectedness have intensified since the new government came to power. Parliament and cabinet members highlight the importance of cutting NHS waiting times and optimising prevention programmes to enable people to stay healthy and economically active. What seems to be less discussed – at least for now – is how the fundamental drivers of poor health and health inequalities will be tackled and to what extent the NHS can contribute to this goal.

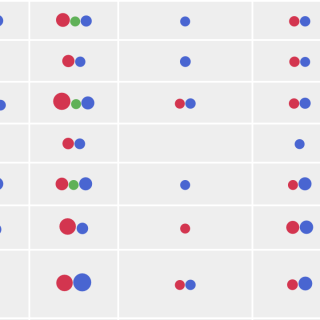
Exploring the impact of dispensing practices on equity in NHS payments to general practices
General practices serving the most deprived populations receive less funding per weighted patient than those serving the least deprived. Here we show that this inequality is driven by a higher concentration of dispensing practices in more affluent areas.

What does the latest GP Patient Survey tell us about socio-economic inequalities in general practice?
Overall patient satisfaction with general practice has improved slightly according to the GP Patient Survey 2024, but remains substantially lower than pre-pandemic levels. Patient satisfaction is not the same across the country. Read more to understand inequalities in patient satisfaction from the latest data.

What works: Finding ways to better support people who frequently attend emergency departments
People who visit emergency departments more frequently than the average often experience multiple socioeconomic difficulties and health problems. In this brief we summarise evidence on how health care services can better support these patients. Meeting these patients’ needs requires an integrated approach that cuts across different health care services but may also involve local authorities and the voluntary sector.
