What are health inequalities?
Health inequalities are the systematic, avoidable and unfair differences in health outcomes that can be observed:
- between populations,
- between social groups within the same population,
- as a gradient across a population ranked by social position. (McCartney 2019)
Health inequalities in the UK have been well documented over the last 50 years, but in recent years we have seen a widening of these inequalities.
They encompass both health outcome inequalities, such as inequalities in mortality and morbidity, and health care inequalities, such as inequalities in access and experience.
Primary care is not immune to inequalities; there are persistent inequalities in funding (practices in socio-economically disadvantaged areas get less funding), workforce and workload.
What causes health inequalities?
Fundamentally we believe that inequalities arise through the unequal distribution of structures within society.
- An unequal distribution of the wider determinants of health, such as income, wealth, education, employment and housing, lead to health outcome inequalities.
- An unequal distribution of the structural determinants of health care, such as workload, workforce and funding, lead to health care inequalities.
What is health equity and how can we achieve it?
Health equity is the absence of health inequalities. Over years of experience and research, we have identified three key approaches to addressing health inequalities.
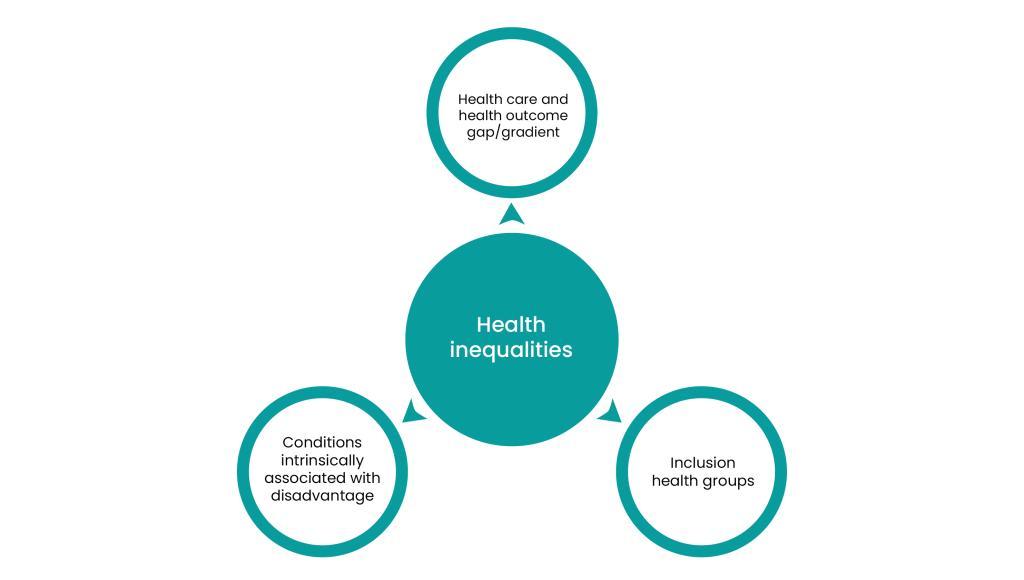
1. Closing the gap or flattening the gradient
Policy-makers and practitioners can target differences between groups or along a socio-economic gradient. These may be differences at an individual level, such as in the management of risk factors, diagnosis or treatment, or at a system level, such as in funding or workforce distribution.
2. Targeting conditions and risk factors intrinsically associated with disadvantage
There are a number of conditions and risk factors which are intrinsically associated with disadvantage. These conditions and risk factors are patterned in a way that practitioners and policy-makers know that by addressing these conditions and risk factors they will be supporting individuals facing disadvantage. The conditions and risk factors include smoking, obesity, alcohol and drug addiction, severe mental illness and tuberculous.
3. Targeting people whose life circumstances put them at risk of poor health
There are a number of groups who are at risk of poor health because of their life circumstances. These groups are often called inclusion health groups and include people who are homeless, street-based sex workers, people seeking asylum, refugees and those with justice service involvement.
