What works: Achieving equitable lipid management

Cardiovascular disease is a leading cause of death in the UK, particularly impacting socioeconomically disadvantaged and ethnic minority groups. Primary care services have a significant role to play in mitigating inequalities in lipid management within health care. This evidence brief examines the available evidence on inequalities across the NHS England cholesterol pathway.
What works: achieving equitable lipid management[PDF 207kb]
Download documentSummary
Cardiovascular disease (CVD) is a leading cause of death in the UK, particularly impacting socioeconomically disadvantaged and ethnic minority groups. Optimal lipid management is crucial for preventing severe morbidity and mortality related to CVD, with programmes like the NHS Long Term Plan and the Core20PLUS5 framework emphasising its importance. However, despite efforts to improve treatment, inequalities persist, with a significant proportion of CVD patients not receiving optimal care, particularly among minority ethnic groups and those in socioeconomically disadvantaged areas.
Whilst recognising the critical importance of wider public health efforts on CVD prevention, primary care services have a significant role to play in mitigating inequalities in lipid management within health care. Evidence on inequalities across the cholesterol pathway suggests that improvements can be achieved with the optimal use of patient registers in disease management and systematic flagging of patients at risk, as well as with multifaceted interventions in three areas:
- Identification and empowerment of disadvantaged patients at risk through culturally tailored screening programmes led by community coalitions and education for primary care professionals to address implicit biases and health inequalities.
- Optimisation of treatment with quality improvement interventions focusing on lifestyle changes, medication, and community health worker support for training and patient care.
- Intensification of treatment to help disadvantaged patients reach cholesterol goals with structured coaching models, regular risk assessments, evidence-based therapeutic choices, patient engagement, and practitioner adherence to national guidelines.
Current challenges
Cardiovascular disease (CVD) remains a major cause of mortality and driver of health inequalities in the UK [1]. According to the latest data from the British Heart Foundation, in 2019 more than 160,000 people died of CVD of which more than 43,000 were under 75 years old [2]. People living in the most socioeconomically disadvantaged regions in England face nearly four times the risk of dying prematurely of CVD compared with those in the least deprived areas. Moreover, CVD prevalence is higher among men, older individuals, those with severe mental illnesses, and people of South Asian or African Caribbean descent [3]. Literature suggests that tackling these inequalities requires co-ordinated public health efforts targeting structural drivers like food insecurity [4] and ‘obesogenic environments’ [5], measures that will mitigate the impact of financial hardship on poorer households [6] together with equitable primary care services [7].
Raised low density lipoprotein (LDL) cholesterol is one of the key risk factors for the development of CVD as it is associated with heart attack, stroke, need for bypass surgery, and death. However, it can be lowered with a combination of lifestyle changes and optimal pharmacological treatment [8] when individuals’ genetic profiles and socioeconomic circumstances allow. A modelling study based on data from the Health Survey for England analysed changes in observed mean total cholesterol levels in the adult England population between 1991–92 (baseline) and 2011–12. The findings showed that during the study period mean total cholesterol declined from 5.86 mmol/L (95% CI: 5.82–5.90) to 5.17 mmol/L (95% CI: 5.14–5.20) and that statins were responsible for almost a third of this reduction. The reduction was found to be greater among the more deprived groups [9][10].
Optimal lipid management especially for people with increased risk of CVD is therefore crucial for the prevention of severe morbidity and mortality. In 2019, the NHS Long Term Plan acknowledged CVD as the single biggest area where the NHS can save lives over the next 10 years [11]. Later, the Core20PLUS5 framework for reducing health inequalities identified optimal lipid management as one of the five clinical areas that require accelerated improvement [12].
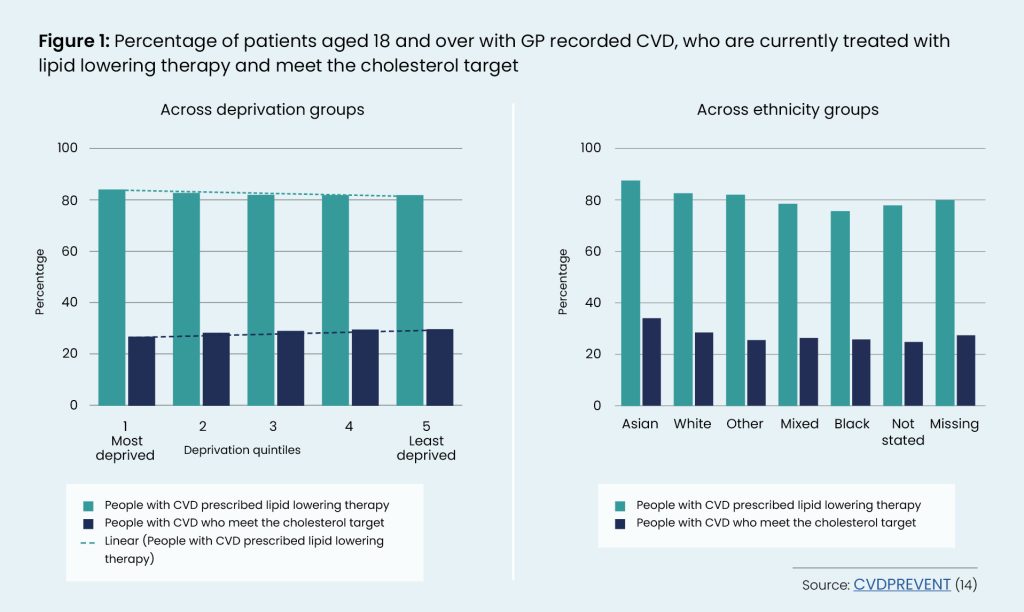
However, researchers have recently estimated that across England almost 20% of people with CVD do not receive optimal treatment. Reducing by only 111,410 patients (almost 5%) has the potential to prevent more than 6,500 CVD events and 805 related deaths in three years [13]. CVD PREVENT data highlights that minority ethnic groups and people with recorded CVD from socioeconomically deprived areas are more likely to be treated with lipid lowering therapy (LLT) but still have higher cholesterol levels [14].
This evidence hints at the important role of the social determinants of health [7][15]. It also suggests that there may be inequalities across the cholesterol pathway [16] due to, for example, inefficient diagnosis and/or treatment of hypercholesterolaemia [17] or culturally inappropriate lifestyle advice for ethnic minority patients [18].
The cholesterol pathway in primary prevention (19) involves assessing CVD risk, discussing lifestyle changes and addressing modifiable risk factors for CVD, assessing for secondary causes of dyslipidaemia, and offering lipid modification therapy, most commonly statins, to those at increased risk of CVD. A great emphasis is put on patient engagement and patient-centred shared decision making. People with established CVD are advised to start lipid modification therapy for secondary prevention, using high intensity statins unless contra-indicated [20]. GP practices are supported in their work on lipid management through QOF incentives [20] and digital tools (lipid management searches) that support patient identification and management [21].
The evidence that follows summarises what works in reducing inequalities across the cholesterol pathway in primary care.
Summary of evidence
Using our evidence maps, we identified 18 studies exploring what works in reducing inequalities in optimal lipid management; seven were either a systematic or a rapid review and eleven were primary studies. Evidence was organised across the different points of the NHS England cholesterol pathway as following:
- Identification and empowerment of disadvantaged patients at risk.
- Optimisation of treatment.
- Intensification of treatment to help disadvantaged patients reach cholesterol goals.
Identification and empowerment of disadvantaged patients at risk
A systematic review [22] examined to what extent engaging community representatives in collaborations with multi-sector private and public organisations to identify common health issues, design programs, and interventions can reduce health inequalities affecting racial and ethnic minority groups. Based on 58 studies, the authors concluded that such initiatives are likely to connect service providers with communities in beneficial ways for individuals and care delivery systems. One of the US reviewed studies based on survey data of 22 communities across 5 years showed decreased racial and ethnic disparities in cholesterol screening between intervention communities and the total population, and decreased disparities related to education level within intervention communities [23]. The intervention was delivered to four ethnic minority groups and concerned the formation of funded community coalitions which designed, implemented and evaluated community driven strategies to eliminate disparities in cardiovascular disease. The logic model of the coalition included capacity building by working with local or state health departments, universities or research organisations to address health issues; targeted actions ranging from community-wide campaigning to screening events; and community and system change in terms of social determinants of health to reduce barriers of access to healthcare.
Another systematic review of primary prevention of cardiovascular disease in indigenous populations in Australia showed that to improve routine risk assessment a holistic approach which encompasses environmental health, justice, housing and psychosocial wellbeing which embraces local and cultural perceptions of health is needed [24]. The review included 19 descriptive, mixed methods, audits or intervention studies. Finally, a study conducted in a large setting of university clinics in the US with 18,757 patients showed that intensive focused education regarding implicit biases and health inequalities among clinicians can reduce inequalities in lipid screening and treatment with ethnic minority patients at risk of CVD being more likely to get tested and treated with statins [25].
Optimisation of treatment
A systematic review of community-based health workers (CHWs) interventions to improve chronic disease management and care among vulnerable populations identified five studies showing a positive impact on lipid management [26]. The studies were conducted in the US and targeted populations combining ethnic minority background (African American or Hispanic) and low socioeconomic status. Studies’ samples ranged from more than 300 up to 869 participants. The authors concluded that the involvement of CHWs can promote cholesterol reduction. Three of the studied interventions focused on primary prevention and aimed to encourage changes in nutrition, especially salt and fat intake, and physical activity [27][28][29]. They used multilingual CHWs who delivered culturally tailored educational sessions and support attending to the diet and exercise habits of the group alongside expert advice and/or small group sessions.
The other two studies focused on secondary prevention and aimed at the optimisation of medication and lifestyle modifications to improve adherence to treatment [30][31]. In both studies, CHWs played a supportive and empowering role alongside counselling, monitoring and prescribing offered by other primary care practitioners. The reviewed literature shows that involving community workers should be one aspect of multifaceted interventions as it is likely to increase acceptability of interventions among marginalised communities [32] and impact behaviour changes [33]. Moreover, a rapid review of interventions to tackle health inequalities in cardiovascular risks for socioeconomically disadvantaged populations confirms that existing evidence concerns a large variety of interventions of different components but does not offer adequate guidance on which of those interventions or their components are effective in optimising lipid management [34]. The conclusions were based on 19 primary studies conducted in Organization for Economic Co-operation and Development (OECD) countries.
Further, an equity-oriented systematic review of quality improvement (QI) strategies in primary care to reduce inequalities in diabetes care identified 30 randomized trials that reported on cholesterol outcomes. An innovative diabetes symptom awareness and self-management educational programme led to significant reductions in total cholesterol and LDL cholesterol in a repeated measures randomized controlled trial with 72 Mexican Americans [35]. Significant reductions in cholesterol and triglycerides were also found in a randomised controlled trial with 79 Korean American immigrants who received structured psychobehavioural education, home glucose monitoring with teletransmission, and bilingual nurse telephone counselling [36]. A telemedicine management was also effective in reducing cholesterol levels among Medicare recipients living in medically underserved areas in New York as shown in a randomised controlled trial with 1665 participants [37]. Finally, a ‘reminder’ and ‘reminder plus feedback’ intervention which utilised computerised systems to produce physician reminders showed an improvement for LDL cholesterol in a trial with 4,138 African American patients [38].
Intensification of treatment to help disadvantaged patients reach cholesterol goals
A clinical trial conducted also in the US with socioeconomically disadvantaged Latinx and African American populations showed that health coaching delivered by trained bilingual medical assistants can help patients achieve cholesterol goals. Coaching involved a structured model of supporting patients inside and outside examination rooms to understand their situation, engage in action plans, manage and adhere to their medication, adopt lifestyle changes and address social determinants of health. Additionally, it involved closely working with the broader care team, taking notes during visits and advocating for patients’ agenda [39]. Committing to structured models and guidelines that involve the periodic assessment of patients was highlighted as a beneficial factor for achieving cholesterol targets by another clinical trial conducted in the Netherlands with hard-to-reach populations living in deprived neighbourhoods [40]. Further, transferable evidence from the EQUALISE study suggests that the extent to which health care practitioners follow national guidelines can be affected by their own biases, so educational interventions that tackle biases can be a useful intervention to help disadvantaged patients achieve cholesterol targets [41].
Finally, a recent study explored the utility of machine learning to cholesterol-lowering pharmacotherapy in 48,226 patients registered across six general practices in South London. The findings show that machine learning data-science analytics can contribute to the identification of suboptimal cholesterol-lowering prescribing, identification of patients who could benefit from more intensified therapy, and recommending evidence-based therapeutic options aligned with national guidelines [42].
Transferable evidence
Transferable evidence from the EQUALISE study suggests that consistent data collection on patients’ ethnicity and socioeconomic position and keeping patients’ records up to date with accurate contact details are key for reducing inequalities in the identification and management of disadvantaged patients at high risk of CVD [7]. Further, the FAIRSTEPS study has shown that systematic flagging of patients’ records to identify those who may be vulnerable to inequalities in health prevention (eg health checks) is a useful and feasible way to reduce inequalities in health outcomes [43].
Limitations
Evidence discussed in this brief comes largely from systematic and rapid reviews on cardiovascular disease conducted in the mid-2010s which means that recent literature has not been considered. The studies discussed do not adopt a common definition of disadvantaged populations, with targeted populations often combining minority ethnic background and low socioeconomic status. Most of the discussed evidence focuses on what works in improving lipid management related outcomes among disadvantaged groups but does not offer measurable indicators of the impact of such interventions on the range of inequalities, nor on how primary care interventions can address social determinants of health.
What works: key recommendations
The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) [44] framework has been adopted to grade the quality of the evidence and support recommendations. The following recommendations focus on primary care although we acknowledge that reducing inequalities in lipid management and CVD risk requires co-ordinated public health initiatives and policy change to address social determinants of health and the structural drivers of inequalities.
| Recommendation | Target audience | GRADE certainty |
| Recommendations from the cholesterol management literature |
||
| A multi-component approach is needed to address inequalities in cholesterol management and should include some or all of the following: | Practices/PCNs/ ICBs | ⊕ ⊕ ⊕ ⊕
High |
|
Practices/ PCNs/ ICBs/ Nationally | ⊕ ⊕ ⊕
Moderate |
|
Practices/ PCNs/ ICBs/ Nationally | ⊕ ⊕ ⊕
Moderate |
|
Practices/PCNs/ ICBs | ⊕ ⊕ ⊕
Moderate |
|
Practices/PCNs/ ICBs | ⊕ ⊕ ⊕
Moderate |
|
Practices/PCNs/ ICBs | ⊕
Very low |
| Recommendations from transferrable equity-focused literature | ||
| Consider flexible approaches to cholesterol management, such as location of service and appointment times, across the prevention pathway to support patients who are unable to follow a standard pathway (evidence from EQUALISE study). | Practices/PCNs/ ICBs | ⊕ ⊕
Low |
| Use equity-focused quality improvement principles to improve overall cholesterol management in addition to addressing inequalities (see our complementary guide on How to undertake Equity-Focused Quality Improvement). | Practices/PCNs/ ICBs | ⊕ ⊕
Low |
|
Practices should consider flagging patient records to identify patients with high cholesterol and vulnerable to cardiovascular disease (see evidence from FAIRSTEPS) (43) |
Practices | ⊕ ⊕
Low |
*The recommendations echo the inclusive and community-centred principles for equitable general practice identified in the EQUALISE study.
Patient voice
Two members of the Health Equity Evidence Citizens’ Panel shared their own experiences.
“My diagnosis happened as a result of a short stay in hospital for chest pain. At that time there was only a history of congenital heart defects in my mother and my twin sister. I was given statins and received yearly blood tests. In 2014, I was given two stents in my right coronary artery, as it was totally blocked. As time has passed my statin dose was increased to the maximum dose. My husband’s story was totally different. His sister had a stroke and it was discovered she had very high cholesterol. She advised my husband to get his checked. We both went to see his Royal Air Force doctor and explained about his sister. The doctor thought that the chance of him having high cholesterol was small. We insisted that he be tested. The results showed we were right to insist as his cholesterol was very high, worryingly so. He was put on statins and checked yearly.”
“It is frightening to realise that close family relatives have died from CVD, and know that lipid monitoring and management may have prevented the early loss of life. I consider myself fortunate to know about familial hypercholesterolaemia. My mother had a heart attack and an emergency triple bypass surgery at the age of 52. It was a shock. I am 56 and have been on statins to lower lipid levels for 12 years.
Achieving health care equity is important to provide those most at risk of CVD, with a care pathway that identifies and addresses the multiple intersecting barriers they face. I am fortunate to have a GP who – considering my family history – has monitored my lipid levels and treated me with medication. However, I can effectively communicate and share my insight and convey my needs, not everyone is equally able to do so. Familial hypercholesterolaemia went undetected across two maternal generations, despite multiple, untimely CVD deaths. Education at community and system level is crucial to promote early intervention through lipid monitoring. For me, timely access through primary care detected early onset of CVD, and effective monitoring and treatment have been crucial for my health. Lipid testing saves lives and reduces the burden on healthcare systems. Prevention is better than a cure.”
How this brief was produced
What is the Living Evidence Map on what works to achieve equitable lipid management in primary care?
Using AI-powered software called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles that examine interventions to address inequalities. The evidence map contains systematic reviews, umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
Useful links
Suggested citation
Gkiouleka A, Dehn Lunn A, Clark E, Torabi P, Cajria C, Blythe J, Kaur S, Moonesinghe J, Ford J. ‘What works – Achieving Equitable Lipid Management’, Evidence Brief, Health Equity Evidence Centre, 2024
References
- Raleigh V, Jefferies D, Wellings D. Cardiovascular disease in England [Internet]. 2022 [cited 2024 Sep 4].
Available from: https://assets.kingsfund.org.uk/f/256914/x/ed99b2b14b/cardiovascular_disease_in_england_2022.pdf - Cheema KM, Dicks E, Pearson J, Samani NJ. Long-term trends in the epidemiology of cardiovascular diseases in the UK: insights from the British Heart Foundation statistical compendium. Cardiovasc Res. 2022 Jun 15;118(10):2267–80.
- Waterall J. Health matters: preventing cardiovascular disease. Public Health Matters Public Health Engl. 2019;
- Chang R, Javed Z, Taha M, Yahya T, Valero-Elizondo J, Brandt EJ, et al. Food insecurity and cardiovascular disease: Current trends and future directions. Am J Prev Cardiol. 2022;9:100303.
- Public Health England. England’s poorest areas are fast food hotspots. 2018.
Available from: https://www.gov.uk/government/news/englands-poorest-areas-are-fast-food-hotspots#:~:text=New%20figures%20from%20PHE%20show,in%20England’s%20most%20deprived%20communities.&text=New%20figures%20from%20Public%20Health,than%20in%20the%20most%20affluent - Jin K, Neubeck L, Atherton I. Impact of area deprivation on the cardiac mortality in the UK between1991 and 2010: evidence from a population-based longitudinal study. Eur J Cardiovasc Nurs. 2021 Jun 1;20(5):436–44.
- Gkiouleka A, Wong G, Sowden S, Bambra C, Siersbaek R, Manji S, et al. Reducing health inequalities through general practice. Lancet Public Health. 2023;8(6):e463–72.
- Penson PE, Pirro M, Banach M. LDL-C: lower is better for longer—even at low risk. BMC Med. 2020 Oct 8;18(1):320.
- Kypridemos C, Bandosz P, Hickey GL, Guzman-Castillo M, Allen K, Buchan I, et al. Quantifying the contribution of statins to the decline in population mean cholesterol by socioeconomic group in England 1991-2012: a modelling study. PLoS One. 2015;10(4):e0123112.
- Wu R, Williams C, Zhou J, Schlackow I, Emberson J, Reith C, et al. Long-term cardiovascular risks and the impact of statin treatment on socioeconomic inequalities: a microsimulation model. Br J Gen Pract. 2024;74(740):e189–98.
- NHS. The NHS Long Term Plan [Internet]. 2019 [cited 2024 Sep 4].
Available from: https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf - NHS England. Core20PLUS5 (adults) – an approach to reducing healthcare inequalities [Internet]. 2021 [cited 2024 Oct 4].
Available from: https://www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement-programme/core20plus5/ - UCL Partners Health Innovation. Size of the Prize – Helping the NHS to Prevent Heart Attacks and Strokes at Scale [Internet].
Available from: https://uclpartners.com/project/size-of-the-prize-for-preventing-heart-attacks-and-strokes-at-scale/ - NHS Benchmarking Network. CVDPrevent [Internet]. 2023 [cited 2024 Oct 4].
Available from: https://www.nhsbenchmarking.nhs.uk/cvdpreventlanding - Jilani MH, Javed Z, Yahya T, Valero-Elizondo J, Khan SU, Kash B, et al. Social determinants of health and cardiovascular disease: current state and future directions towards healthcare equity. Curr Atheroscler Rep. 2021;23:1–11.
- Daiichi Sankyo UK Ltd, HEART UK. Closing the cholesterol gap. Putting high cholesterol at the heart of action on health inequalities [Internet]. 2022 May [cited 2024 Oct 4].
Available from: https://www.daiichi-sankyo.co.uk/fileadmin/daiichi-sankyo-contents/DS_UK/Downloads/About_Us/Closing_the_cholesterol_gap_report.pdf - Schofield J, Kwok S, France M, Capps N, Eatough R, Yadav R, et al. Knowledge gaps in the management of familial hypercholesterolaemia. A UK based survey. Atherosclerosis. 2016 Sep 1;252:161–5.
- Grace C, Begum R, Subhani S, Kopelman P, Greenhalgh T. Prevention of type 2 diabetes in British Bangladeshis: qualitative study of community, religious, and professional perspectives. Bmj. 2008;337.
- Khatib R, Neely D. Summary of national guidance for lipid management for primary and secondary prevention of CVD.”. Natl Inst Health Care Excell.
- NHS England. Improving lipid management to reduce cardiovascular disease and save lives [Internet]. 2023 [cited 2024 Oct 4].
Available from: https://www.england.nhs.uk/long-read/improving-lipid-management-to-reduce-cardiovascular-disease-and-save-lives/ - NHS England. Lipid management searches [Internet]. 2024 [cited 2024 Oct 4].
Available from: https://digital.nhs.uk/services/lipid-management-searches - Anderson LM, Adeney KL, Shinn C, Safranek S, Buckner‐Brown J, Krause LK. Community coalition‐driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Syst Rev. 2015;(6).
- Liao Y, Tucker P, Siegel P, Liburd L, Giles WH, Investigators R 2010. Decreasing disparity in cholesterol screening in minority communities—Findings from the racial and ethnic approaches to community health 2010. J Epidemiol Community Health. 2010;64(4):292–9.
- Merone L, McDermott R, Mein J, Clarke P, McDonald M. Primary Prevention of Cardiovascular Disease in Minority Indigenous Populations: A Systematic Review. Heart Lung Circ. 2020 Sep 1;29(9):1278–91.
- Umer M, Kalra D, Rai SN, Rai S, Wu X, Vorla M, et al. Equitable Access to Screening and Lipid-Lowering Therapies in a Large Academic Center after Educational Interventions. J Clin Lipidol. 2023;17(4):e14–5.
- Kim K, Choi JS, Choi E, Nieman CL, Joo JH, Lin FR, et al. Effects of Community-Based Health Worker Interventions to Improve Chronic Disease Management and Care Among Vulnerable Populations: A Systematic Review. Am J Public Health. 2016 Apr 1;106(4):e3–28.
- Balcazar HG, Byrd TL, Ortiz M, Tondapu SR, Chavez M. A randomized community intervention to improve hypertension control among Mexican Americans: using the promotoras de salud community outreach model. J Health Care Poor Underserved. 2009;20(4):1079–94.
- Balcázar HG, de Heer H, Rosenthal L, Duarte MO, Aguirre M, Flores L, et al. Peer reviewed: a Promotores de Salud intervention to reduce cardiovascular disease risk in a high-risk Hispanic border population, 2005-2008. Prev Chronic Dis. 2010;7(2).
- Lynch EB. A self-management intervention for African Americans with comorbid diabetes and hypertension: a pilot randomized controlled trial. Prev Chronic Dis. 2014;11.
- Allen JK, Himmelfarb CRD, Szanton SL, Bone L, Hill MN, Levine DM. COACH trial: a randomized controlled trial of nurse practitioner/community health worker cardiovascular disease risk reduction in urban community health centers: rationale and design. Contemp Clin Trials. 2011;32(3):403–11.
- Becker DM, Yanek LR, Johnson Jr WR, Garrett D, Moy TF, Reynolds SS, et al. Impact of a community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation. 2005;111(10):1298–304.
- Chapman J, Qureshi N, Kai J. Effectiveness of physical activity and dietary interventions in South Asian populations: a systematic review. Br J Gen Pract. 2013;63(607):e104–14.
- Verhagen I, Steunenberg B, de Wit NJ, Ros WJ. Community health worker interventions to improve access to health care services for older adults from ethnic minorities: a systematic review. BMC Health Serv Res. 2014 Nov 13;14(1):497.
- Fu Y, Yu G, Maulana N, Thomson K. Interventions to tackle health inequalities in cardiovascular risks for socioeconomically disadvantaged populations: a rapid review. Br Med Bull. 2023;148(1):22.
- García AA, Brown SA, Horner SD, Zuñiga J, Arheart KL. Home-based diabetes symptom self-management education for Mexican Americans with type 2 diabetes. Health Educ Res. 2015 Jun 1;30(3):484–96.
- Kim MT, Han HR, Song HJ, Lee JE, Kim J, Ryu JP, et al. A Community-Based, Culturally Tailored Behavioral Intervention for Korean Americans With Type 2 Diabetes. Diabetes Educ. 2009 Nov 1;35(6):986–94.
- Shea S, Weinstock RS, Teresi JA, Palmas W, Starren J, Cimino JJ, et al. A Randomized Trial Comparing Telemedicine Case Management with Usual Care in Older, Ethnically Diverse, Medically Underserved Patients with Diabetes Mellitus: 5 Year Results of the IDEATel Study. J Am Med Inform Assoc. 2009 Jul 1;16(4):446–56.
- Phillips LS, Ziemer DC, Doyle JP, Barnes CS, Kolm P, Branch WT, et al. An endocrinologist-supported intervention aimed at providers improves diabetes management in a primary care site: improving primary care of African Americans with diabetes (IPCAAD) 7. Diabetes Care. 2005;28(10):2352–60.
- Willard-Grace R, Chen EH, Hessler D, DeVore D, Prado C, Bodenheimer T, et al. Health coaching by medical assistants to improve control of diabetes, hypertension, and hyperlipidemia in low-income patients: a randomized controlled trial. Ann Fam Med. 2015;13(2):130–8.
- Fakiri FE, Bruijnzeels MA, Uitewaal PJM, Frenken RAA, Berg M, Hoes AW. Intensified preventive care to reduce cardiovascular risk in healthcare centres located in deprived neighbourhoods: a randomized controlled trial. Eur J Cardiovasc Prev Rehabil. 2008 Aug 1;15(4):488–93.
- Gkiouleka A, Wong G, Sowden S, Kuhn I, Moseley A, Manji S, et al. Reducing health inequalities through general practice: a realist review and action framework. Health Soc Care Deliv Res. 2024;12(7).
- Krentz AJ, Haddon-Hill G, Zou X, Pankova N, Jaun A. Machine Learning Applied to Cholesterol-Lowering Pharmacotherapy: Proof-of-Concept in High-Risk Patients Treated in Primary Care. Metab Syndr Relat Disord. 2023 Oct 1;21(8):453–9.
- Jackson B, Ariss S, Burton C, Coster J, Reynolds J, Lawy T. The FAIRSTEPS Study: Framework to Address Inequities in pRimary care using STakEholder PerspectiveS—short report and user guidance. 2023.
- Siemieniuk R, Guyatt G. What is GRADE. BMJ J Best Pract. 2019;10:77–85.