What works: Addressing inequalities in the primary and secondary outpatient interface

An estimated 15 million GP appointments are used every year dealing with issues between primary and secondary care. A dysfunctional primary-secondary care interface is likely to widen health inequalities by disproportionately impacting underserved populations. This evidence brief examines the evidence and provides recommendations on what works to reduce inequalities at the primary-secondary care interface.
What works: Addressing inequalities in the primary and secondary outpatient interface[PDF 218kb]
Download documentSummary
An estimated 15 million GP appointments are used every year dealing with issues between primary and secondary care. A dysfunctional primary-secondary care interface impacts on patient experience, safety and staff workload, and is likely to widen health inequalities by disproportionately impacting underserved populations. The NHS has had numerous initiatives to improve this interface. While the aim is often to increase efficiency, short-term efficiency gains may be outweighed by populations missing out on care and subsequently presenting late and acutely.
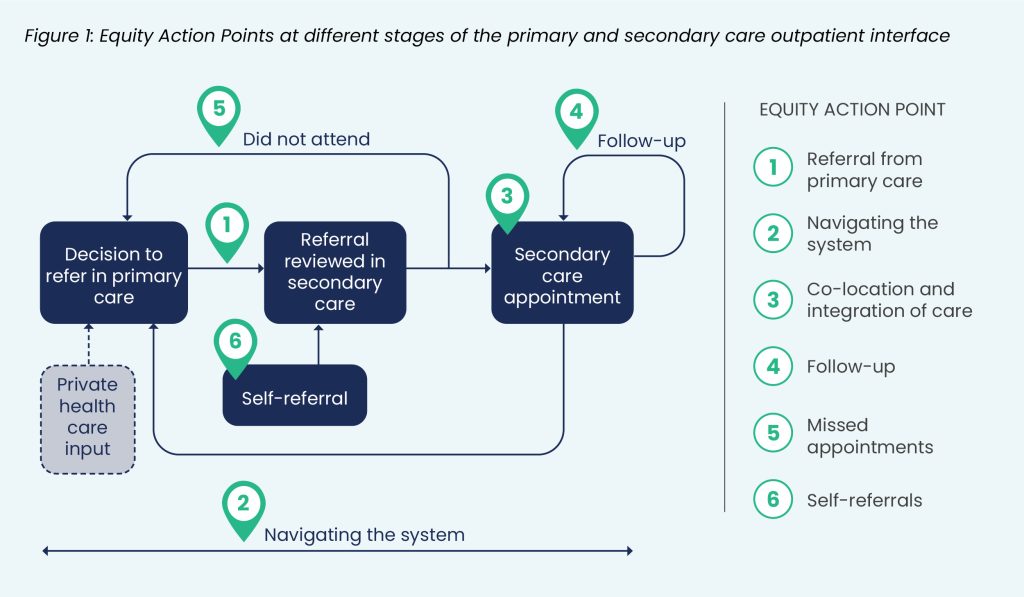
There is little evidence examining strategies at the outpatient interface to support disadvantaged groups. Inequalities can arise at multiple points from referral to follow-up. Based on our evidence, we recommend support mechanisms to help attendance at specialist appointments, care coordinators, inclusive and culturally competent communication, flexibility, co-location where possible and using patient-initiated follow up on a case-by-case basis. We also need better evaluation that understands the distribution of impacts across different communities.
Current challenges
The medical interface is described as “the point of interaction between different systems… where a patient journey crosses from one area of care into another such as moving between primary and secondary care, between health and social care and between scheduled and unscheduled care” [1].
The primary and secondary care outpatient interface is a two-way relationship that encompasses referrals (and re-referrals) from general practice to secondary and community care specialists; communication relating to patient care, screening and investigations; management of did-not-attends (DNAs); and medication management. Problems can arise at any point along the pathway.
Issues at the primary and secondary care outpatient interface have been recognised as an important problem for many years, impacting on patient experience of care, safety, and staff workload and morale. Managing issues regarding the interface between primary and secondary care is estimated to consume 15 million GP appointments annually [2]. Healthwatch England polls demonstrated that one in five patients seeking specialist care found themselves in a ‘referral black hole’; referred to the wrong service, removed from a waiting list, had an appointment cancelled or lacking referral follow-up [2]. There is frustration amongst UK GPs around interface issues between primary and secondary care [3]. Inability to access timely specialist care can lead to worsening health and avoidable admissions and requests from secondary care for GPs to refer to other specialists can add delays and increase administrative burden [4]. For disadvantaged population groups delayed specialist care increases rates of hospital presentation disproportionately compared to the general population, perpetuating health inequalities [5].
Attempts to address some of the issues around the primary-secondary care interface have been implemented, with the 2017 standard contract [6] and subsequent guidance from the British Medical Association and the Academy of Medical Royal Colleges delineating professional responsibilities across the patient pathway [7][8]. In many areas, Advice and Guidance (A&G) services have been introduced to help GPs get rapid advice from a specialist, however the A&G process can add barriers to referral or delays if specialists’ capacity is limited. The Academy of Medical Royal Colleges has many examples of good practice, but only one mention of inequalities [8].
The NHS’ vision for community diagnostic centres (CDC) is to help tackle health care inequalities by moving health care closer to home. 160 centres are planned by the end of 2024 building on learning from successes of the Covid vaccine rollout to deliver health care closer to home. There is as yet inadequate evidence of the impact of CDCs on health care inequalities.
Here we focus on how to address inequalities in the primary and secondary outpatient interface.
Summary of evidence
Evidence assessing how interventions at the interface between primary and secondary care impact inequalities is limited. We have drawn upon this literature and complementary guiding principles to develop evidence-informed recommendations (see figure 1).
Equity Action Point 1: Referral from primary care
Patients from the most deprived areas have a higher rate of outpatient appointments than patients from the least deprived areas [9], which reflects the high burden of ill health amongst patients from lower socioeconomic backgrounds. Programmes to improve referral patterns from primary care include the use of locally designed pathways, decision-support tools and advice and guidance from secondary care clinicians without formal referral. There is relatively little evidence on the impact of these schemes on health inequalities.
A service development project aimed to improve the quality and effectiveness of secondary care referrals made by GPs in Wales [10]. GPs from ten of 13 practices with high rates of multi-morbidity and deprivation participated in regular discussions with local hospital specialists to assess the appropriateness of referrals and compatibility with local guidelines. Overall referral rates fell from 5.5 to 4.3 (per 1000 patients per quarter) and variation in individual GP referral rates also narrowed (from 2.6-7.7 to 3.0-6.5 per 1000 patients per quarter). GPs’ self-assessment of referral quality also improved on average from 89% to 95%. Despite the relatively small size and the absence of a control group, it provides preliminary support that referral management improves quality and reduces unwarranted variation at the primary and secondary care interface.
A before-and-after study in Brazil assessed the impact of introducing E-consultations between the referring GP and an external medical attendant auditing the referral [11]. Conversations aimed to define the need, triage category and most appropriate destination of the referral or support clinicians to manage cases in primary care. The integration of telehealth into referral management systems reduced the number of cases waiting for specialised care between January 2019 and February 2020 across three socioeconomically disadvantaged regions by 89%, 77% and 55%. The median waiting time was also reduced.
Equity Action Point 2: Navigating the system
As a result of the pandemic, access to planned care fell more drastically in the most deprived areas of the UK compared to the least deprived [12]. The King’s Fund identified that a waiting time of 12 months or more was twice as common for patients living in the most deprived parts of England compared to those in the least deprived areas [13]. Unsurprisingly, duration of time spent on an outpatient waiting list was linked with worse outcomes. This association disproportionately impacts already disadvantaged patients, exacerbating inequalities. Kulkarni et al evaluated the impact of deprivation for patients on lengthy waiting lists, identifying that those patients in the most deprived areas reported longer symptom duration, more severe pain, lower quality of life, poorer overall health and lower activity levels [12].
Care coordinators support people to navigate the health and care system, providing a point of continuity and support for patients across services, particularly for patients with multiple long-term conditions, and those living with frailty [14]. They have been found to have positive impacts on health outcomes, including improved mental health symptoms, reduced nursing home admissions, reduced rehospitalisation rates and improved quality of life measures [15][16][17][18]. There is little evidence around targeted use of care coordination to support people experiencing health inequalities. A scoping review of the access to health care for people experiencing homelessness in the UK and Ireland highlighted issues around referral processes, discharge planning, fragmentation of services and poor communication with the use of care coordinators, for example specialist nurses, showing positive impacts [19].
Equity Action Point 3: Co-location and integration of care
Co-location of primary and specialist care has been proposed as a potential strategy for improving integration of health care. A systematic review and meta-analysis found mixed results for the impact of placing specialty care alongside primary care [20]. Meta-analysis of three randomised controlled trials (RCTs) comprising over 2000 patients demonstrated significant improvements in patient satisfaction with co-location of behavioural and mental health services with primary care (OR 3.16, CI 95% 1.49 to 6.68). The impact of integrated care on other outcomes was inconsistent between studies. The pooled odds ratios of two RCTs (OR 0.39, CI 95% 0.33 to 0.45) and an additional observational study (OR 0.15, CI 95% 0.07 to 0.34) found a reduction in depression severity in patients accessing co-located behavioural health care. However, no statistically significant reduction in depression severity resulted from the same intervention for a further five RCTs (OR 0.70, CI 95% 0.41 to 1.18). A single cross-sectional study involving 813 patients with HIV attending integrated infectious disease and primary care services did not demonstrate any increase in service uptake associated with co-location [21].
A systematic review examining the efficacy and cultural acceptability of integrated care for health care delivery to indigenous Americans found increased continuity of care, improved cultural acceptability of care, easier access to mental health services and reduced rates of depression [22]. An Australian systematic review evaluated integrated specialist and primary care services, including 10 studies [23]. Of the total 7697 patients included in the review, those described as being from disadvantaged population groups were 2495 patients in a semi-rural region and 40 Aboriginal Australians. The authors found that integrated primary-secondary care, compared to usual care, can improve elements of disease control and service delivery at a modestly increased cost, although the reported impact on clinical outcomes was limited. A further review of an integrated diabetes service involving specialist outreach for 124 Aboriginal Australians across three remote communities demonstrated improvement in baseline HbA1c and total cholesterol [24].
Equity Action Point 4: Follow-up
Patient-initiated follow-up (PIFU) has been proposed as a mechanism of matching available services with patient need [25]. By allowing patients to schedule their care as and when they deem necessary, PIFU intends to reduce the incidence of missed, cancelled and unnecessary appointments. The NHS is rolling out PIFU to increase capacity in outpatients [26]. A rapid evidence review conducted by the Nuffield Trust revealed that there is very little existing research on how PIFU may impact health inequalities [25]. Of the 15 studies which examined PIFU, most focused on low-risk patients with higher levels of agency to initiate contact. Eight showed a statistically significant reduction in outpatient appointments compared to fixed follow-up and seven showed no difference. There was little or no effect on clinical outcomes. Previous research suggests that services which require more patient effort are more likely to increase inequalities as those with high health literacy and more resources are more likely to benefit [27].
Equity Action Point 5: Missed appointments
Did-not-attend (DNA) rates are disproportionately high in lower socioeconomic status groups, with patients in the lowest two deprivation quintiles being the most likely to DNA appointments [28][29][30]. Elderly patients, those with mental illness and minority ethnic groups also demonstrate higher rates of DNAs [28]. Data from Scotland shows that patients who miss GP appointments are more likely to miss hospital appointments and be higher users of inpatient and outpatient hospital care, but not emergency department care [31].
A community mental health team in Enfield, the 64th most deprived local authority district in the UK, implemented the use of text message reminders to reduce DNA rates [32]. Overall clinic DNA rates reduced from 11.4% to 10.6% during a six month period. When broken down by discipline, non-attendance for patients with medical follow-up improved most significantly, reducing from 17.7% to 11.8%. While multiple studies support the use of text message reminders to mitigate non-attendance rates across the NHS, most do not disaggregate results by population groups [28]. A large retrospective and prospective study examined the implementation of text message reminders at a new patient breast clinic in North-West England and found reduced DNA rates from 8.2% to 4.1% (p<0.001) during the January 2019 to March 2020 trial period [33]. However, median age of non-attending patients rose between the pre-intervention and post-intervention cycle from 38 years-old to 47 years-old (p<0.001), indicating the intervention was much less effective for elderly patients.
In their literature review of the causes, impacts and methods to mitigate DNA rates, Wilson et al conclude that reducing non-attendance rates equitably will not be achieved by a “one size fits all” approach [28]. Letter prompts to improve clinic attendance were trialled by a community mental health clinic in Leeds covering 64,000 patients from predominantly deprived backgrounds [34]. 1433 brief paper prompts were distributed to all patients with scheduled appointments between June and November 2007. Non-attendance dropped to 17% during the trial period, a statistically significant reduction in comparison to clinic DNA rates of 26%. Reminder calls proved effective at reducing DNA rates in a randomised controlled trial involving 393 patients, however DNAs from patients from socioeconomically disadvantaged backgrounds remained higher than their affluent counterparts (61% versus 46%) [35].
Equity Action Point 6: Self-referrals
Please see our existing evidence brief here. In summary, based on a review of 19 studies, we found evidence that generally, self-referral services tend to be used more by higher socioeconomic groups, white groups, women, and young populations, although these patterns were not consistent in every context. There was little evidence for what works to reduce these inequalities and a paucity of evidence examining language barriers in self-referral pathways.
Other considerations
Impact of private health care
There is an increasing interaction between primary care and private providers as the use of private health care increases. Private health care largely focuses on specialist consultations, diagnostics and elective care. Its expansion increases inequalities, with those able to pay being able to get access to quicker advice, diagnosis and management. It raises questions about the impact on the NHS when private health care use generates additional tasks for NHS staff, such as arranging blood tests, providing prescriptions or referrals. The BMA has produced guidance to support general practice to reduce the workload burden associated with private health care use (36). There is a lack of data on the administrative burden of private health care on the NHS and subsequent impact on the ability to deliver core services.
Digital support for patients
The NHS app launched in 2019 aiming to be a trustworthy and branded digital channel for patients to find health information and access NHS services. Individuals not registered with a GP practice or who do not have both telephone and internet access are unable to access the range of NHS app services. Age, socioeconomic status and disability are key predictors of digital exclusion (37). As well as access challenges, e-health literacy rates are disproportionately low in underserved populations and app-based health care may contribute to widening inequalities if not considered from a system perspective.
Key recommendations
The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) framework has been adopted to grade the quality of the evidence and support recommendations.
Given the relative lack of evidence-based interventions to reduce inequalities at the primary-secondary care interface, we have also drawn on the broader principles of the EQUALISE study to inform these recommendations. These principles are
- Connected: Interventions and services should be understood, designed, and delivered as connected components of coordinated action against health inequalities.
- Intersectional: Care should adopt an intersectional perspective to account for the different impact of services and interventions among patients according to their circumstances and experience of (multiple) disadvantage.
- Flexible: Care delivery should be flexible enough to make allowances for different patient needs and preferences in terms of time, accessible communication, location, and provided support.
- Inclusive: We need to cultivate an organisational culture that is less western-centric and normative to ensure that people are not excluded due to wrong assumptions about who they are, what they need, and how they ‘should’ behave.
- Community-centred: Everybody involved in care should have a say in how it is conceived, (re)designed, and delivered including clinical and non-clinical members of staff, patients, and their networks.
| Recommendation | Target audience | GRADE certainty |
| Referral from primary care |
||
|
Adopt, with caution, Advice and Guidance (A&G) and referral management schemes to guide primary care providers’ decision making; ensure evaluation addresses impact on health inequalities
|
Practices/ Secondary care providers/ ICBs |
⊕
Very low |
| Ask about barriers to attendance and highlight potential financial support for eligible patients, such as the NHS healthcare travel costs scheme, at the point of referral (recommendation based on EQUALISE study evidence) | Practices | ⊕
Very low |
| Highlight patient’s communication needs (eg language, digital exclusion) and potential barriers to attendance in referrals, such as transport, caring responsibilities, lack of flexibility around work patterns (recommendation based on EQUALISE study evidence) | Practices | ⊕
Very low |
| Navigating the system |
||
| Implement targeted care coordination to support patients and carers to navigate the healthcare system | Practices/ PCNs | ⊕ ⊕
Low |
| Develop inclusive, culturally competent means of communicating with patients who are waiting, taking into account language barriers, digital inclusion, and other factors (eg people who are homeless may not have a dependable postal address) | Secondary care providers | ⊕ ⊕
Low |
|
Co-location and integration of care
|
||
| Offer flexibility around appointment modes (face-to-face/remote) and timings (eg evenings/weekends) targeted at disadvantaged groups (recommendation based on EQUALISE study evidence) | Secondary care providers | ⊕
Very low |
|
Where possible, health systems should co-locate services and diagnostics with better integration of care prioritised to areas of high socioeconomic deprivation
|
ICBs | ⊕ ⊕
Low |
| Follow-up |
||
|
Use patient-initiated follow-up with caution and on a case-by-case basis because it is likely that people from higher socioeconomic groups will use it more. Where used, there should be shared decision making between clinician and patient, taking into account socioeconomic factors and a safety net process |
Secondary care providers | ⊕ ⊕
Low |
|
Missed appointments
|
||
| Use targeted appointment reminders such as text message, letter and phone call reminders | Secondary care providers | ⊕ ⊕
Low |
| Offer further appointments to patients who miss appointments rather than asking their practice to re-refer. Ask patients what would support them to attend in future (recommendation based on EQUALISE study evidence) | Secondary care providers | ⊕ ⊕
Low |
| Evaluate missed appointments from a health inequalities perspective and develop with targeted support for patients where there are greatest barriers to attendance | Secondary care providers/ ICBs | ⊕
Very low |
|
Self-referrals
|
||
|
For recommendations on self-referrals, please see our evidence brief here |
Not applicable | Not applicable |
Summary of how the brief was produced
What is the Living Evidence Map on What Works to address health inequalities in primary care?
Using AI-powered software, called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles which examine interventions to address inequalities. The evidence map contains systematic review and umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
Suggested citation
Dehn Lunn A, Lynch H, Adam B, Blythe J, Clark E, Engamba S, Torabi P, Ford J. Evidence brief: What works – Addressing inequalities in the primary and secondary outpatient interface. Health Equity Evidence Centre; 2024.
References
- David Landau SP. Policy Exchange. London; 2023 [cited 2023 Mar 12]. Medical Evolution: Measures to improve the interface between primary and secondary care.
Available from: https://policyexchange.org.uk/wp-content/uploads/Medical-Evolution.pdf - Healthwatch. ‘Referrals black hole’ – new findings of people’s experiences of GP referrals [Internet]. 2023.
Available from: https://www.healthwatch.co.uk/blog/2023-02-16/referrals-black-hole-new-findings-peoples-experiences-gp-referrals - GPs call for action on work transfer from hospitals to tackle workload crisis [Internet]. [cited 2024 Mar 18].
Available from: https://www.gponline.com/article/1827035 - Workload transfer in the NHS: The Great British Dump – BJGP Life [Internet]. 2023 [cited 2024 Mar 18].
Available from: https://bjgplife.com/workload-transfer-in-the-nhs-the-great-british-dump/ - Miler JA, Carver H, Masterton W, Parkes T, Maden M, Jones L, et al. What treatment and services are effective for people who are homeless and use drugs? A systematic ‘review of reviews.’ PLoS One. 2021;16(7):e0254729.
- NHS England » The interface between primary and secondary care: Key messages for NHS clinicians and managers [Internet]. [cited 2024 Mar 18].
Available from: https://www.england.nhs.uk/publication/the-interface-between-primary-and-secondary-care-key-messages-for-nhs-clinicians-and-managers/ - The British Medical Association is the trade union and professional body for doctors in the UK. [Internet]. 2023 [cited 2024 Mar 18]. Primary and secondary care interface.
Available from: https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/primary-and-secondary-care/primary-and-secondary-care-working-together - Academy of Medical Royal Colleges. General practice and secondary care Working better together. 2023.
- Asaria M, Doran T, Cookson R. The costs of inequality: whole-population modelling study of lifetime inpatient hospital costs in the English National Health Service by level of neighbourhood deprivation. J Epidemiol Community Health. 2016 Oct 1;70(10):990–6.
- Evans E, Aiking H, Edwards A. Reducing variation in general practitioner referral rates through clinical engagement and peer review of referrals: a service improvement project. Qual Prim Care. 2011;19(4):263–72.
- Gadenz SD, Basso J, de Oliviera PRBP, Sperling S, Zuanazzi MVD, Oliveira GG, et al. Telehealth to support referral management in a universal health system: a before-and-after study. BMC Health Serv Res. 2021 Sep 25;21(1):1012.
- Kulkarni K, Shah R, Mangwani J, Dias J. The impact of deprivation on patients awaiting planned care. Bone Jt Open. 2022;3(10):777–85.
- Robertson R. Tackling health inequalities on NHS waiting lists-Learning from local case studies. 2023.
- NHS England » Care co-ordinators [Internet]. [cited 2024 Mar 18].
Available from: https://www.england.nhs.uk/personalisedcare/workforce-and-training/care-co-ordinators/ - Archer J, Bower P, Gilbody S, Lovell K, Richards D, Gask L, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev [Internet]. 2012 [cited 2024 Mar 18];(10).
Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006525.pub2/full - Newcomer R, Maravilla V, Faculjak P, Graves MT. Outcomes of preventive case management among high-risk elderly in three medical groups: a randomized clinical trial. Eval Health Prof. 2004 Dec;27(4):323–48.
- Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166(17):1822–8.
- Hawkins K, Parker PM, Hommer CE, Bhattarai GR, Huang J, Wells TS, et al. Evaluation of a High-Risk Case Management Pilot Program for Medicare Beneficiaries with Medigap Coverage. Popul Health Manag. 2015 Apr 1;18(2):93–103.
- McNeill S, O’Donovan D, Hart N. Access to healthcare for people experiencing homelessness in the UK and Ireland: a scoping review. BMC Health Serv Res. 2022 Jul 13;22(1):910.
- Elrashidi MY, Mohammed K, Bora PR, Haydour Q, Farah W, DeJesus R, et al. Co-located specialty care within primary care practice settings: A systematic review and meta-analysis. In Elsevier; 2018. p. 52–66.
- Momplaisir F, Mounzer K, Long JA. Preventive cancer screening practices in HIV-positive patients. AIDS Care. 2014;26(1):87–94.
- Lewis ME, Myhra LL. Integrated care with Indigenous populations: considering the role of health care systems in health disparities. J Health Care Poor Underserved. 2018;29(3):1083–107.
- Mitchell GK, Burridge L, Zhang J, Donald M, Scott IA, Dart J, et al. Systematic review of integrated models of health care delivered at the primary–secondary interface: how effective is it and what determines effectiveness? Aust J Prim Health. 2015;21(4):391–408.
- Hotu C, Rémond M, Maguire G, Ekinci E, Cohen N. Impact of an integrated diabetes service involving specialist outreach and primary health care on risk factors for micro‐and macrovascular diabetes complications in remote Indigenous communities in Australia. Aust J Rural Health. 2018;26(6):394–9.
- Reed S, Crellin N. Patient-initiated follow-up: will it free up capacity in outpatient care. Nuffield Trust. 2022;
- NHS England,. 2022/23 priorities and operational planning guidance. 2022.
- Gkiouleka A, Wong G, Sowden S, Bambra C, Siersbaek R, Manji S, et al. Reducing health inequalities through general practice. Lancet Public Health. 2023 Jun 1;8(6):e463–72.
- Wilson R, Winnard Y. Causes, impacts and possible mitigation of non-attendance of appointments within the National Health Service: a literature review. J Health Organ Manag. 2022;36(7):892–911.
- England NHS. Reducing did not attends (DNAs) in outpatient services [Internet]. 2023.
Available from: https://www.england.nhs.uk/long-read/reducing-did-not-attends-dnas-in-outpatient-services/ - NHS Health Scotland,. Who is least likely to attend? An analysis of outpatient appointment ‘Did Not Attend’ (DNA) data in Scotland. 2015.
- ‘Missingness’ in health care: Associations between hospital utilization and missed appointments in general practice. A retrospective cohort study | PLOS ONE [Internet]. [cited 2024 Mar 18].
Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0253163 - Filippidou M, Lingwood S, Mirza I. Reducing non-attendance rates in a community mental health team. BMJ Open Qual. 2014;3(1):u202228. w1114.
- Kiruparan P, Kiruparan N, Debnath D. Impact of pre-appointment contact and short message service alerts in reducing ‘Did Not Attend’(DNA) rate on rapid access new patient breast clinics: a DGH perspective. BMC Health Serv Res. 2020;20(1):1–9.
- Jayaram M, Rattehalli RD, Kader I. Prompt letters to reduce non-attendance: applying evidence based practice. BMC Psychiatry. 2008;8:1–6.
- McLean SM, Booth A, Gee M, Salway S, Cobb M, Bhanbhro S, et al. Appointment reminder systems are effective but not optimal: results of a systematic review and evidence synthesis employing realist principles. Patient Prefer Adherence. 2016 Apr 4;10:479–99.
- The British Medical Association is the trade union and professional body for doctors in the UK. [Internet]. 2023 [cited 2024 Mar 18]. General practice responsibility in responding to private healthcare.
Available from: https://www.bma.org.uk/advice-and-support/gp-practices/managing-workload/general-practice-responsibility-in-responding-to-private-healthcare - Ueno A, Dennis C, Dafoulas GA. Digital exclusion and relative digital deprivation: Exploring factors and moderators of internet non-use in the UK. Technol Forecast Soc Change. 2023 Dec 1;197:122935.
Related resources

What works: Mitigating inequalities in patient self-referral to specialist services
Self-referral of patients directly to specialist services may help relieve pressure from GPs; however, concerns have been raised that this may increase inequalities. This brief presents recommendations to mitigate the potential of self-referral to increase inequalities.