What works: Health and care interventions to support people from disadvantaged backgrounds in returning to work

Return to work interventions seek to address long-term work or sickness absence, but whether they achieve equitable outcomes is unclear. This brief reviews the evidence to identify health and care interventions that support people from disadvantaged backgrounds return to employment.
What works: Health and care interventions to support people from disadvantaged backgrounds in returning to work[PDF 321kb]
Download documentSummary
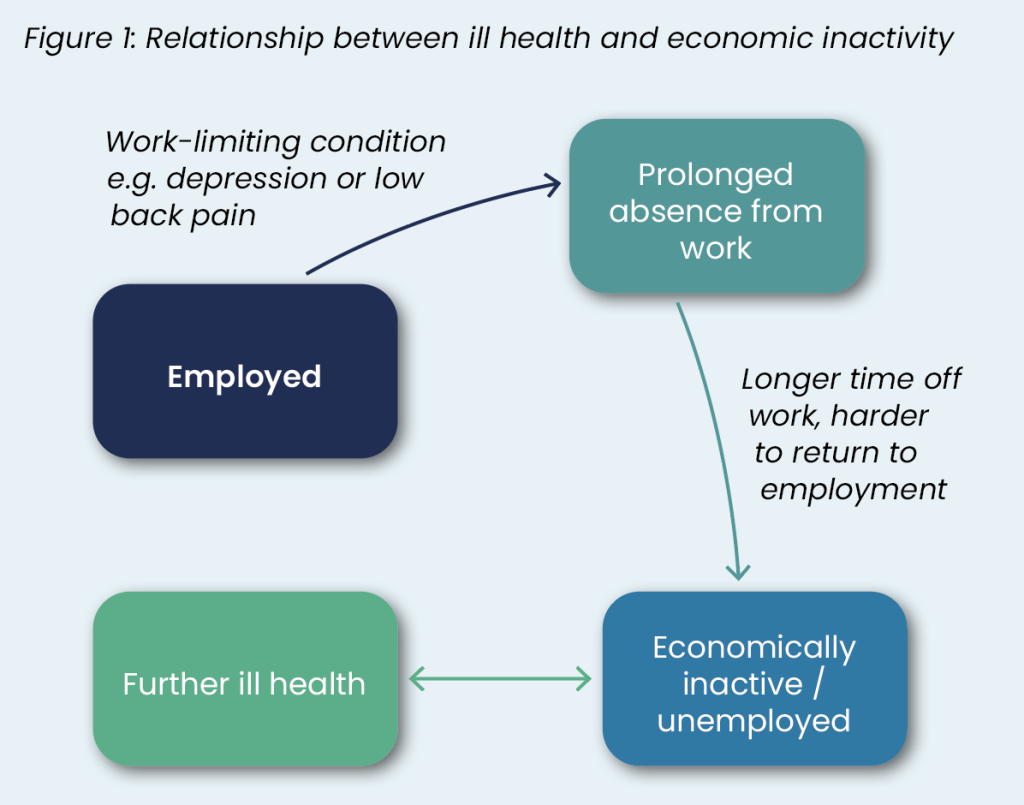
Employment, while being a marker of economic growth and productivity, is also a wider determinant of health. Disadvantaged groups have higher rates of work-limiting conditions which is compounded by poorer access to health and care interventions. Return to work (RTW) interventions seek to address long-term work or sickness absence, but whether they achieve equitable outcomes is unclear.
We reviewed evidence across 57 studies to determine health and care interventions that support people from disadvantaged backgrounds return to employment. RTW interventions varied in both design and target population and rarely sought to address the needs of disadvantaged groups. Generally, effective interventions were multicomponent, multidisciplinary, involved the workplace, and for some conditions, were individualised. Based on the evidence, to optimise RTW for disadvantaged groups, programmes should be:
- Holistic and adapted using the biopsychosocial model, tailored approaches, and cultural sensitivity.
- Multicomponent with collaboration between health services and the workplace, advocacy for reasonable adjustments, and work-focused psychological therapies.
- Multidisciplinary with RTW coordinators and referral to non-health care services such as supported employment.
Current challenges
Decades of research has proven the correlation between employment and better health outcomes. UK studies have found higher rates of self-reported poor health and mental wellbeing in economically inactive and precariously employed people compared to those fully- employed [1][2]. A comparative study across 34 European countries including the UK showed that unemployment is associated with poorer health for both men and women, regardless of national welfare provision [3].
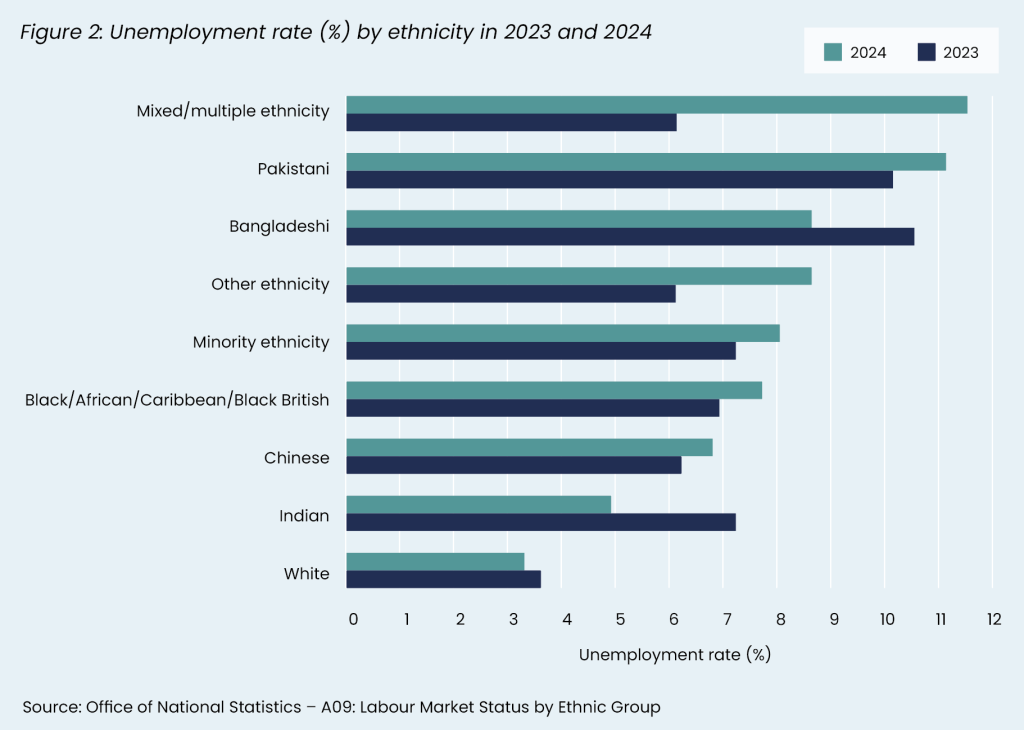
Economic inactivity rates in the UK have been slowly declining in the last decade, with 21.7% of people aged 16 to 64 being economically inactive as of August to October 2024 [4]. Results from the 2022 Annual Population Survey revealed that Pakistani and Bangladeshi ethnic groups combined had the highest rate of economic inactivity (33%) [5], possibly explained by higher prevalences of work-limiting conditions seen in these groups [6]. Furthermore, data from the 2024 Labour Force Survey revealed that people with Multiple/Mixed ethnicity, as well as Pakistani and Bangladeshi ethnicities, had higher rates of unemployment compared to other ethnic groups (Figure 2) [6], despite unemployment rates being the lowest they have been since the COVID-19 pandemic [7].
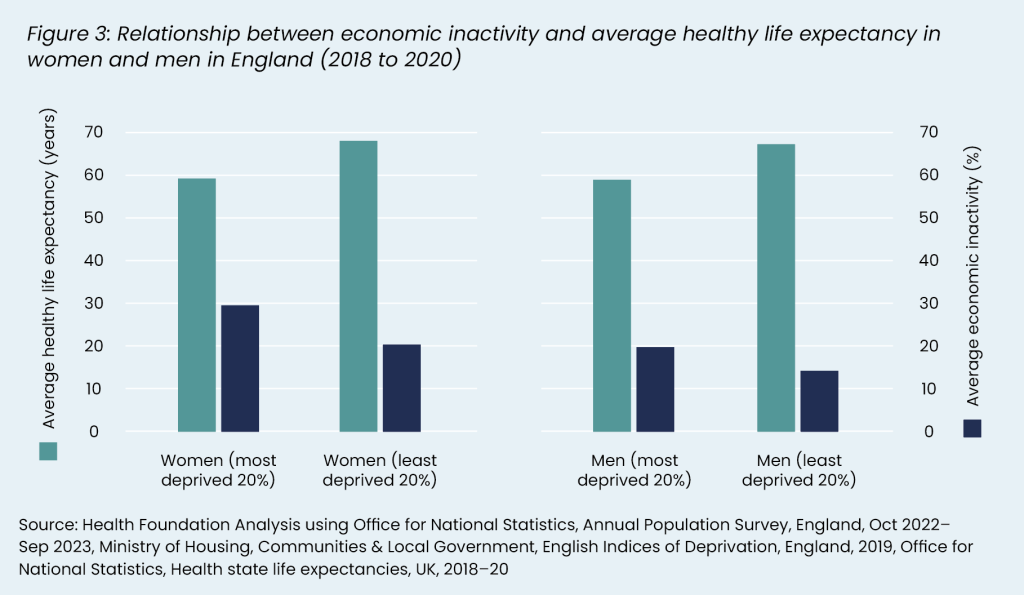
Women and men from the most deprived areas also suffer from lower healthy life expectancy rates and higher rates of economic inactivity compared to their least deprived counterparts [8] (Figure 3). Women in the UK also have higher rates of sickness absence, and evidence shows that the longer an employee’s sickness absence lasts, the less likely they are to return to work [9][10][11].
The NHS is the largest employer in the UK. Almost 1 in 20 NHS staff were off work due to sickness absence in August 2024, with the most common reason being mental health reasons, closely followed by back problems and other musculoskeletal problems [12]. Mental health accounted for 28.5% of all sickness absence in that time period, increasing from 26.3% the month before [12].
Here, we review the evidence of RTW programmes to support groups disproportionately affected by being out of work. RTW is an outcome measure used to describe the process in which an individual is supported towards full recovery to recommence employment. It typically reflects a person re-entering the workforce after a period of work or sickness absence, though some researchers advocate RTW more broadly include productivity of the employee and the quality and satisfaction of the work [13][14].
Definitions
Return to work: The process by which an individual is supported towards full recovery to recommence employment. It typically reflects a person re- entering the workforce after a period of work or sickness absence.
Working-age population: Those aged 16 to 64 years old.
Unemployment: People without a job, who have been actively seeking work in the past four weeks and are available to start work in the next two weeks. Or people out of work who have found a job and are waiting to start it in the next two weeks.
Economically inactive: People not in employment who have not been seeking work within the last four weeks and/or are unable to start work within the next two months.
Long-term health condition: A condition that lasts for 12 months or more.
Source: Office for National Statistics
Summary of evidence
We prioritised 57 of the most relevant and robust studies from 90 systematic reviews of RTW interventions identified through a search of MEDLINE. Recent evidence shows inequalities in the RTW process for minority ethnic groups [15][16]. However, there is a lack of evidence on the underlying reasons for differences in RTW outcomes across characteristics such as age, sex, ethnicity, or levels of socioeconomic deprivation.
Overall, RTW interventions were mostly targeted to people of working-age and with four major conditions: 1) mental health, 2) musculoskeletal (MSK), 3) cancer and 4) brain injury (either acquired through stroke or traumatic). Most studies examined RTW for people with mental health conditions. There were limited RTW reviews focusing on those with acute complications of long-term chronic conditions (such as post coronary event in the setting of cardiovascular disease, or flare-up of inflammatory bowel disease).
RTW interventions ranged from psychological interventions to physical activity, including workplace and recreational interventions. Interventions were also delivered by professionals from multiple disciplines, ranging from allied health specialists to job coaches hired external to health care settings.
The effectiveness of RTW interventions varied according to condition and context. For example, supported employment interventions appeared to be better suited to people with mental health conditions. Overall, RTW interventions were more likely to be successful across all population groups if they were, in order of the most supporting evidence: 1) multicomponent, 2) workplace-related, 3) multidisciplinary, and 4) person-centred.
Health care organisations play an important role in supporting people to return to work and there is evidence that early involvement of workplace is essential for successful RTW. A review of 95 studies by the Swedish Agency for Health Technology Assessment [17] looked at health care RTW interventions in the case of long-term sick leave and found that, across both single and multicomponent interventions, those that involved some type of workplace contact or workplace coordination activity had a positive effect on RTW in the short term (12 months), particularly with sick leave associated with mental health or MSK conditions. While the certainty of the evidence was low, it is supported by findings from many reviews that demonstrate that workplace involvement, whether it be through liaising with employers or modifying the workplace, is better for RTW outcomes [18]–[24].
For the health care setting, we found that RTW programmes worked better for disadvantaged groups if they were:
1. Holistic and culturally adapted, focusing on:
- Biopsychosocial model of care
- Tailored approaches
- Culturally sensitive RTW programmes
2. Multicomponent, focusing on:
- Reasonable adjustments
- Work-focused psychological therapies
3. Multidisciplinary, focusing on:
- RTW coordinators
- Referral to non-health care services, such as supported employment.
In the following paragraphs we discuss these components in greater detail, and we conclude with a summary of cost-effectiveness for some of the interventions discussed.
1. Holistic and culturally adapted RTW programmes
Biopsychosocial model of care
Returning to the workplace is a complex process that requires intervention components to holistically address the clinical, occupational, and psychosocial factors keeping people off work. Ideally, this process should be informed by theoretical models that underpin the value of the interactions between the person and the workplace. Evidence has consistently found that psychosocial factors have an independent effect on RTW outcomes [25] and the biopsychosocial (BPS) model (see definitions box) is widely recognised across reviews to be the most appropriate and effective approach to RTW intervention design, particularly for people with musculoskeletal conditions [26]–[32]. Designing RTW programmes from a BPS perspective is promising for disadvantaged individuals because it is more likely to account for the psychosocial factors these people uniquely experience in their effort to recover and return to work. While we did not find evidence to demonstrate the impact of RTW interventions using the BPS model on disadvantaged groups specifically, we know that acknowledging psychosocial pathways can reduce health inequalities [33].
Definition: Biopsychosocial Model [34] Initially conceptualised and developed by George Engel in 1977, the biopsychosocial model has been refined over the years to be defined as a model of care that appreciates the complex, circular relationship between mind, body, and environment. The model views health and illness as shaped by psychosocial factors beyond their biomedical explanation [35], incorporating an understanding of how culture, economic status, health literacy, self-effiacy, and beliefs and norms impact health outcomes.
Tailored and person-centred approaches
While the RTW evidence base was mixed regarding the optimal method of delivery for RTW interventions (i.e. individual vs group), researchers emphasised the importance of ensuring at a minimum that interventions are person-centred [34]–[37]. A qualitative review of 97 studies [38] found that patients’ needs for work-focused health care covered four themes including a tailored approach. Tailored approaches to RTW included: flexibility in work-focused health care, attention for the personal situation, inclusion of individual goals, and disease-specific information in relation to work [38].
Two reviews examining RTW in people with acquired brain injury found that tailored, person-centred approaches were often more successful [24][39]. A review of 57 studies by Murray and colleagues [39] looking at the use of vocational rehabilitation (VR) found that VR that emphasised tailoring to the individual by considering the interaction between the client, stakeholders, work tasks, and environment was often more successful.
Culturally sensitive RTW programmes
An integrative review augmented with focus groups by Coutu and colleagues explored ethnocultural factors influencing sustainable RTW. The authors found that, first, belonging to a minority ethnic group was associated with cumulative risk factors, such as low educational levels and/or manual work; and second, for people who have recently immigrated, differences between the prevailing workplace culture of the host country and workers’ reference points can negatively affect RTW due to miscommunication, trust issues and conflicting values [16]. They suggested strategies including the use of a ‘cultural humility’ model to help promote different cultures without one dominating the other. Cultural humility helps health care workers to recognise structural factors that may compound RTW progress and has been described extensively in Canadian occupational health literature [40][41].
Jetha and colleagues’ review [15] looking at racial and ethnic inequities in RTW also suggested anti- racist approaches to work disability management. Anti-racist models of care adopted across all organisational levels, either through staff cultural competency training or meaningful involvement of marginalised groups through leadership, can address structural challenges faced by minority ethnic groups in the RTW process [42].
These findings echo broader evidence suggesting that cultural adaptation is a key component of interventions that can effectively address the needs of disadvantaged groups as demonstrated in detail in our evidence brief: What works to improve access, uptake, and optimisation of behavioural interventions in health care settings to better meet the needs of disadvantaged groups [43]. Given that ethnic minorities are more likely to be diagnosed with certain conditions such as prostate cancer [44] or to be diagnosed at a later stage (e.g., ethnic minority women with breast cancer) [45] delivering culturally tailored RTW programmes is necessary to ensure that these programmes will be effective for those who need them the most.
2. Multi-component RTW interventions
RTW interventions with multiple components appear to better address biopsychosocial factors than single component interventions. For example, Cullen and colleagues [18] looked at the effectiveness of 36 workplace RTW interventions for both mental health and MSK conditions, and found that most effective interventions included the following components: a health-focused work component, service coordination and reasonable adjustments [46]. They found that interventions encompassing at least two components were more effective, which is also supported by Nowrouzi and colleagues [47] and Mikkelsen and colleagues [48].
Multicomponent interventions were also effective among people with different conditions, including individuals post road traffic collisions [49] and those with chronic pain [50]. Wegrzynek and colleagues [50], across 16 trials, found that multicomponent interventions had more positive effects compared to cognitive behavioural therapy (CBT) or physical treatments alone. In fact, they found that CBT alone sometimes delayed RTW for some chronic pain sufferers compared to treatment as usual. Similar findings of combining RTW methods were also found in Hult and colleagues’ review [51] regarding health-improving interventions to increase employment in job seekers.
Multiple complementary reviews examining RTW interventions for people living with or recovering from cancer also found that multicomponent interventions were more likely to be effective [52][53][54]. De Boer and colleagues [52] reviewed 15 RCTs looking at psycho-educational, vocational, physical or multicomponent interventions in participants mostly with breast or prostate cancer. They found that both physical and multicomponent interventions were more effective. Their review suggested that multicomponent interventions are likely to help between 69 and 219 per 1000 people with cancer return to work. Cocchiara and colleagues’ umbrella review [53] focusing on RTW programmes for people with breast cancer also found more positive effects in interventions that combined physical activity, counselling and education, and addressed modifiable environmental factors.
Reasonable adjustments
Reasonable adjustments include modifications to the workplace that allow for a safer and more sustainable RTW [46]. An example of a reasonable adjustment is having graded or paced RTW, a type of stepped approach to workplace integration or contact. Mikkelsen and colleagues [48], across 42 RCTs that studied RTW in sick-listed workers due to common mental disorders, stress-related disorders, and other mental health conditions, found moderate evidence for graded RTW compared to standard programmes and therapy alone. Timing and length of interventions did not change the size of effect, and the population group that benefited the most were employees on sickness absence due to stress. Similarly, a study by Cochrane and colleagues [55] suggested that a stepped care approach may be more effective than usual care in facilitating RTW in employees with MSK pain.
Health care professionals can advocate for reasonable adjustments, predominantly through written reports. While it is not a doctor’s role to give advice on the law and define workload concepts within disability, a doctor can comment on the ease or otherwise with which the person they are treating carries out their day-to-day activities that can then inform paced approaches to return to work [56]. Furthermore, recent legislation has expanded the scope of health professionals able to certify fit notes [57]. Referring patients to specialist occupational health assessments performed independently may also be valuable [56][58].
Work-focused psychological therapies
Severe mental illness is higher in more socioeconomically disadvantaged areas [59]. Furthermore, there are known inequalities to both mental health access and quality of mental health care for disadvantaged groups [60]. Therefore, mental health interventions targeted at socioeconomically disadvantaged areas are more likely to support disadvantaged groups.
There is some evidence that adapting psychological therapies, such as CBT and counselling, to be more work-focused improved RTW outcomes compared to standard programmes. Several reviews [21][61]–[65] focusing on working-age people with mental health conditions found such adaptation beneficial. For example, Slater and colleagues [61] assessed the effectiveness of work-focused CBT (W-CBT) in facilitating RTW, and across 23 studies found that it was effective particularly with mild to moderate mental health conditions. W-CBT was defined as CBT that is delivered with ‘an understanding of RTW as the goal’, with components that are always framed ‘by matters, subjects and contexts related to work’ [61]. Brämberg and colleagues [64] also found the same results across 11 European studies (including 8 RCTs) in workers on sick leave due to mental health problems. Their findings showed that W-CBT resulted in increased or faster return to work compared with standard care or no intervention.
Delivering work-focused psychological therapies to areas known to be linked with higher prevalences of mental health conditions may increase access and improve RTW outcomes by targeting service delivery to at-risk populations.
3. Multidisciplinary care
Interventions involving multiple disciplines, both within and outside health and care, were more successful in returning people to work. Evidence consistently shows that multidisciplinary health care teams improve outcomes [66]. Multidisciplinary care is particularly effective and relevant for disadvantaged groups because of multiple compounding BPS issues [67], so the addition of team roles such as a care coordinator, social worker or community health worker can better address these issues [68][69].
Programmes in the reviewed evidence include a diverse range of professionals, from occupational therapists (OTs) to psychiatrists, as well as non- healthcare roles such as vocational counsellors and job coaches. While it is difficult to determine the isolated impact of a single discipline, RTW outcomes generally improved when employees were provided with coordinated, holistic multidisciplinary care [18][19][65][70]. The health and care disciplines most involved in returning people to work which showed positive effects included physiotherapists, OTs, and psychologists [47]–[50][53][62][70]–[75]. Rehabilitation specialists were also present for more complex conditions, such as stroke [39][76][77].
Verhoef and colleagues [70] looked at the effectiveness of 30 multicomponent vocational rehabilitation interventions for workers with chronic physical conditions (excluding chronic back pain), such as rheumatic diseases, musculoskeletal disorders and HIV. They found half applied a monodisciplinary approach and the other half used a multidisciplinary approach, with more high-quality trials showing positive impacts on work status for multidisciplinary programmes. Bernaers and colleagues [20] exclusively studied multidisciplinary interventions (including health professionals from at least two different disciplines) for subacute low back pain, and found that interventions resulted in fewer days of work absence or sick leave, while having benefits in terms of improved pain and functional status in the short term. However, they did not increase the rate at which people returned to work fully, without limitation from pain.
RTW coordinators: providing coordinated care and advocacy
Dol and colleagues [78] systematically reviewed the impact of RTW coordinators on the RTW process for multiple work-limiting conditions, ranging from psychological to MSK conditions. According to the Dol’s review [78], RTW coordinators often have titles such as case managers, disability prevention specialists, or rehabilitation counsellors. They found strong evidence across 14 studies that sickness absence was reduced in duration when employees were given opportunity to have face-to-face contact with a RTW coordinator. Interventions that included training of RTW coordinators along with other key intervention aspects, such as RTW coordinators developing a RTW plan, also had moderate impact on reducing work absence [78]. RTW coordinators may also improve integration between health care teams and help promote cultural sensitivity, alongside having specialised knowledge about workplace processes.
A qualitative review by Hajendijk and colleagues [38] also found the importance of a ‘clear and continuous process’ focusing on early access to support, continuity in support, interdisciplinary teamwork and coordination, and information about rights and regulations – functions that can be provided by a RTW coordinator.
Referral to supported employment and Individual placement support services
Several studies included in our search [79]–[84] found that non-healthcare interventions, such as supported employment, were highly effective, particularly in working-age people with severe mental health conditions. Supported employment is characterised by a ‘place and train’ approach that places an individual in a work setting, with most of the intervention provided in that setting to ensure success in the workplace [85]. Individual placement support (IPS) is a type of supported employment that is highly structured and involves close integration of occupational and health services [86]. Bond and colleagues and de Winter and colleagues [79][80] found IPS to be effective in improving employment outcomes, particularly in young people and in those with severe mental illnesses, such as schizophrenia.
Cost-effectiveness of RTW interventions
Evidence on cost-effectiveness of RTW interventions is in its infancy, with key methodological challenges in part due to various perspectives taken (i.e. health provider versus societal) and huge variability in costs, both direct and indirect. Furthermore, many economic analyses have been undertaken outside the UK which limits the transferability of evidence. The best evidence we found for cost-effectiveness came from two studies [17][87]. In a Swedish review [17] of 95 studies, ten looked at cost-effectiveness of healthcare-based RTW interventions for sick leave. The findings showed a small positive effect on return to work (> 5 days relative reduction in one year per person), though the certainty of this was limited. Dewa and colleagues [87] examined the cost-effectiveness of ten RTW interventions for mental illness-related sickness absence and found that it was highly dependent on the subgroup of employees being targeted, with mixed evidence revealing that the more complex the condition is, the less likely it is for the interventions to be cost- effective.
Limitations
The heterogeneity and variable quality of RTW studies meant that we were limited in making definitive conclusions about what interventions were the most effective. Furthermore, a large majority of studies originated from Scandinavian countries or North America which may limit the generalisability of our findings. There is a clear lack of RTW research around some subgroups of the working-age population, particularly those suffering from acute complications of chronic diseases such as cardiovascular disease and inflammatory bowel disease. Most of the RTW literature did not comment on or provide disaggregated data across different groups based on race or ethnicity, and socioeconomic determinants of health. Therefore, the evidence that we present on what works to support disadvantaged groups in returning to work is limited.
What works: key recommendations
| Recommendation | Target audience | GRADE certainty |
|
RTW programmes should be informed by the biopsychosocial model of care and adopt a holistic and individualised approach. |
NHS England, ICBs, PCNs, Trusts, Occupational health services, community allied health |
⊕ ⊕ ⊕ Moderate |
|
RTW programmes should be culturally tailored to support people from diverse ethnic and cultural backgrounds. |
NHS England, ICBs, PCNs, Trusts, Occupational health services, community allied health and other health disciplines |
⊕ ⊕ ⊕ Moderate |
|
RTW programmes should be multicomponent, containing at least two or more elements, such as work-focused psychological therapies, reasonable workplace adjustments, co-ordination of care and behavioural interventions. |
NHS England, ICBs, PCNs, Trusts, Occupational health services, community allied health and other health disciplines, industry |
⊕ ⊕ ⊕ Moderate |
|
RTW programmes should consider targeting and delivering their services to populations with work-limiting conditions that are linked with disadvantage, such as severe mental illness. |
NHS England, ICBs, PCNs, Trusts, Occupational health services, community allied health and other health disciplines |
⊕ ⊕ Low |
|
RTW programmes should involve multidisciplinary teams, including occupational therapists, psychologists, RTW coordinators and counsellors. |
NHS England, ICBs, PCNs, Trusts, Occupational health services, employers, industry |
⊕ ⊕ ⊕ Moderate |
|
RTW programmes should include improved co-ordination between NHS organisations and employers, such as the use of RTW coordinators. |
NHS England, ICBs, PCNs, Trusts, Occupational health services, employers, industry |
⊕ ⊕ Low |
|
NHS organisations should identify and refer suitable patients to Individual Placement Support schemes, and advocate for workplace modifications, flexible working and phased RTW plans through reasonable adjustments. |
NHS England, ICBs, PCNs, Trusts, Occupational health services, employers, industry |
⊕ ⊕ Low |
|
Health care commissioners should work with cross- government departments to evaluate the economic benefits of RTW across multiple sectors. |
DHSC, NHS England, ICBs, local authorities |
⊕ ⊕ ⊕ Moderate |
*GRADE certainty communicates the strength of evidence for each recommendation.
Recommendations which are supported by large trials will be graded highest whereas those arising from small studies or transferable evidence will be graded lower. The grading should not be interpreted as priority for policy implementation – i.e. some recommendations may have a low GRADE rating but likely to make a substantial population impact.
How this brief was produced
Using AI-powered software called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles that examine interventions to address inequalities. The evidence map contains systematic reviews, umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
This evidence brief was commissioned by NHS England to support their statutory responsibility to deliver equitable health care. Policy interventions beyond health care services were not in scope. DL is funded by NIHR ARC North Thames. The views expressed in this publication are those of the author(s) and not necessarily those of NHS England or NIHR.
Suggested citation
Harasgama S, Lamb D, Kuhn I, Gkiouleka A, Ford J, Wong Y, Gajria C, Loftus L, Dehn Lunn A, Blythe J. Evidence brief: What works – Health and care interventions to support people from disadvantaged backgrounds in returning to work. Health Equity Evidence Centre; 2025
References
- Richards L, Paskov M. Social class, employment status and inequality in psychological well-being in the UK: Cross-sectional and fixed effects analyses over two decades. Soc Sci Med. 2016 Oct 1;167:45–53.
- Emerson E, Hatton C, Baines S, Robertson J. The association between employment status and health among British adults with and without intellectual impairments: cross-sectional analyses of a cohort study. BMC Public Health. 2018 Mar 27;18(1):401.
- Bambra C, Eikemo TA. Welfare state regimes, unemployment and health: a comparative study of the relationship between unemployment and self-reported health in 23 European countries. J Epidemiol Community Health. 2009 Feb 1;63(2):92.
- LFS: Economic inactivity rate: UK: All: Aged 16-64: %: SA – Office for National Statistics [Internet]. [cited 2025 Jan 14]
Available from: https://www.ons.gov.uk/employmentandlabourmarket/peoplenotinwork/economicinactivity/timeseries/lf2s/lms - UK Government. Economic inactivity -Ethnicity Facts and Figures [Internet]. 2023 [cited 2025 Jan 14].
Available from: https://www.ethnicity-facts-figures.service.gov.uk/work-pay-and-benefits/unemployment-and-economic-inactivity/economic-inactivity/latest/#download-the-data - What we know about the UK’s working-age health challenge – The Health Foundation [Internet]
Available from: https://www.health.org.uk/publications/long-reads/what-we-know-about-the-uk-s-working-age-health-challenge - Unemployment rate (aged 16 and over, seasonally adjusted): % – Office for National Statistics [Internet].
Available from: https://www.ons.gov.uk/employmentandlabourmarket/peoplenotinwork/unemployment/timeseries/mgsx/lms - Relationship between employment and health | The Health Foundation [Internet]. [cited 2025 Jan 14]
Available from: Available from: https://www.health.org.uk/evidence-hub/work/employment-and-unemployment/relationship-between-employment-and-health - Marmot M, Allen J, Goldblatt P, Boyce T, McNeish D, Grady M, et al. Fair Society, Healthy Lives: The Marmot Review. 2010;
- Institute of Employment Rights. Institute of Employment Rights. 2024 [cited 2024 Dec 9]. Almost one in ten UK workers increasingly trapped in precarious work
Available from: https://www.ier.org.uk/news/almost-one-in-ten-uk-workers-increasingly-trapped-in-precarious-work/ - Gray B, Grey C, Hookway A, Homolova L, Davies A. Differences in the impact of precarious employment on health across population subgroups: a scoping review. Perspect Public Health. 2021 Jan 1;141(1):37–49.
- NHS England Digital [Internet]. [cited 2025 Jan 17]. NHS Sickness Absence Rates, August 2024.
Available from: https://digital.nhs.uk/data-and-information/publications/statistical/nhs-sickness-absence-rates/august-2024 - Wasiak R, Young AE, Roessler RT, McPherson KM, van Poppel MNM, Anema JR. Measuring Return to Work. J Occup Rehabil. 2007 Dec 1;17(4):766–81.
- Steenstra IA, Lee H, de Vroome EMM, Busse JW, Hogg-Johnson SJ. Comparing Current Definitions of Return to Work: A Measurement Approach. J Occup Rehabil. 2012 Sep 1;22(3):394–400.
- Jetha A, Navaratnerajah L, Shahidi FV, Carnide N, Biswas A, Yanar B, et al. Racial and Ethnic Inequities in the Return-to-Work of Workers Experiencing Injury or Illness: A Systematic Review. J Occup Rehabil. 2023 Sep 1;33(3):432–49.
- Coutu MF, Durand MJ, Coté D, Tremblay D, Sylvain C, Gouin MM, et al. Ethnocultural Minority Workers and Sustainable Return to Work Following Work Disability: A Qualitative Interpretive Description Study. J Occup Rehabil. 2022 Dec 1;32(4):773–89.
- Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU). Health care interventions in case of long-term sick leave: A systematic review and assessment of medical, economic, social and ethical aspects. 2022;
- Cullen K L, Irvin E, Collie A, Clay F, Gensby U, Jennings P A, et al. Effectiveness of Workplace Interventions in Return-to-Work for Musculoskeletal, Pain-Related and Mental Health Conditions: An Update of the Evidence and Messages for Practitioners. J Occup Rehabil. 2018;28(1):1–15.
- Nazarov S, Manuwald U, Leonardi M, Foucaud J, Lamore K, Guastafierro Erika, et al. Chronic Diseases and Employment: Which Interventions Support the Maintenance of Work and Return to Work among Workers with Chronic Illnesses? A Systematic Review. Int J Environ Res Public Health. 2019;16(10)
- Bernaers L, Cnockaert E, Braeckman L, Mairiaux P, Willems TM. Disability and return to work after a multidisciplinary intervention for (sub)acute low back pain: A systematic review. Clin Rehabil. 2023;37(7):964–74.
- Joyce S, Modini M, Christensen H, Mykletun A, Bryant R, Mitchell P B, et al. Workplace interventions for common mental disorders: a systematic meta-review. Psychol Med. 2016;46(4):683–97.
- Lambreghts C, Vandenbroeck S, Goorts K, Godderis L. Return-to-work interventions for sick-listed employees with burnout: a systematic review. Occup Environ Med. 2023;80(9):538–44.
- Tarro L, Llaurado E, Ulldemolins G, Hermoso P, Sola R. Effectiveness of Workplace Interventions for Improving Absenteeism, Productivity, and Work Ability of Employees: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int J Environ Res Public Health. 2020;17(6).
- Donker-Cools B H P M, Daams J G, Wind H, Frings-Dresen M H W. Effective return-to-work interventions after acquired brain injury: A systematic review. Brain Inj. 2016;30(2):113–31
- Cancelliere C, Donovan J, Stochkendahl MJ, Biscardi M, Ammendolia C, Myburgh C, et al. Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropr Man Ther. 2016 Sep 8;24(1):32.
- Garton PL. Benefits of a Structured Biopsychosocial Approach to Workplace Rehabilitation for Musculoskeletal Injury. 2019;
- Schultz IZ, Stowell AW, Feuerstein M, Gatchel RJ. Models of Return to Work for Musculoskeletal Disorders. J Occup Rehabil. 2007 Jun 1;17(2):327–52
- Knauf MT, Schultz IZ, Stewart AM, Gatchel RJ. Models of Return to Work for Musculoskeletal Disorders: Advances in Conceptualization and Research. In: Gatchel RJ, Schultz IZ, editors. Handbook of Musculoskeletal Pain and Disability Disorders in the Workplace. New York, NY: Springer New York; 2014. p. 431–52.
- Duong HP, Garcia A, Hilfiker R, Léger B, Luthi F. Systematic Review of Biopsychosocial Prognostic Factors for Return to Work After Acute Orthopedic Trauma: A 2020 Update. Front Rehabil Sci. 2022;2.
- Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo R, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database Syst Rev. 2014;(9).
- Hochheim M, Ramm P, Amelung V. The effectiveness of low-dosed outpatient biopsychosocial interventions compared to active physical interventions on pain and disability in adults with nonspecific chronic low back pain: A systematic review with meta-analysis. Pain Pract. 2023 Apr 1;23(4):409–36.
- Bartys S, Frederiksen P, Bendix T, Burton K. System influences on work disability due to low back pain: an international evidence synthesis. Health Policy. 2017;121(8):903–12.
- GOV.UK [Internet]. 2017 [cited 2025 Jan 17]. Psychosocial pathways and health outcomes.
Available from: https://www.gov.uk/government/publications/psychosocial-pathways-and-health-outcomes - De Dios Perez B, McQueen J, Craven K, Radford K, Blake H, Smith B, et al. The effectiveness of occupational therapy supporting return to work for people who sustain serious injuries or develop long-term (physical or mental) health conditions: A systematic review. Br J Occup Ther. 2023 Jul 1;86(7):467–81.
- Butow P, Laidsaar-Powell R, Konings S, Lim C Y. S, Koczwara B. Return to work after a cancer diagnosis: a meta-review of reviews and a meta-synthesis of recent qualitative studies. J Cancer Surviv. 2020;14(2):114–34.
- White C, Green RA, Samantha S, Anderson SL, Howe C, Sun J, et al. The Influence of Social Support and Social Integration Factors on Return to Work Outcomes for Individuals with Work-Related Injuries: A Systematic Review. J Occup Rehabil. 2019;29(3):636–59
- Weizhe S, Gholizadeh L, Perry L, Kyoungrim K, Heydari M. Factors associated with return to work following myocardial infarction: A systematic review of observational studies. J Clin Nurs. 2021;30(3–4):323–40.
- Hagendijk ME, Zipfel N, Melles M, van der Wees PJ, Hulshof CTJ, Zwaan E, et al. Patients’ Needs Regarding Work-Focused Healthcare: A Qualitative Evidence Synthesis. J Occup Rehabil. 2024 Jul 25;
- Murray A, Watter K, McLennan V, Vogler J, Nielsen M, Jeffery S, et al. Identifying models, processes, and components of vocational rehabilitation following acquired brain injury: a systematic scoping review. Disabil Rehabil. 2022;44(24):7641–54
- Beagan BL. Approaches to culture and diversity: A critical synthesis of occupational therapy literature: Des approches en matière de culture et de diversité : une synthèse critique de la littérature en ergothérapie. Can J Occup Ther. 2015 Dec 1;82(5):272–82.
- Hammell KRW. Occupation, well-being, and culture: Theory and cultural humility / Occupation, bien-être et culture : la théorie et l’humilité culturelle. Can J Occup Ther. 2013 Oct 1;80(4):224–34.
- Ford J, Harasgama S, Lamb D, Dehn Lunn A, Gajria C, Painter H, et al. Evidence Brief: What works: Empowering health care staff to address health inequalities. Health Equity Evidence Centre; 2024.
- Gkiouleka A, Harasgama S, Pearce H, Kuhn I, Dehn Lunn A, Torabi P, et al. What works: Improving access, uptake and optimisation of behavioural interventions in the health care setting to better meet the needs of disadvantaged groups. Health Equity Evidence Centre; 2024
- Lloyd T, Hounsome L, Mehay A, Mee S, Verne J, Cooper A. Lifetime risk of being diagnosed with, or dying from, prostate cancer by major ethnic group in England 2008–2010. BMC Med. 2015 Jul 30;13(1):171.
- Gathani T, Reeves G, Broggio J, Barnes I. Ethnicity and the tumour characteristics of invasive breast cancer in over 116,500 women in England. Br J Cancer. 2021 Aug 1;125(4):611–7.
- GOV.UK [Internet]. [cited 2024 Dec 2]. Reasonable adjustments for workers with disabilities or health conditions
Available from: https://www.gov.uk/reasonable-adjustments-for-disabled-workers - Nowrouzi B, Garrido P, Gohar B, Yazdani A, Chattu V K, Bani-Fatemi Ali, et al. Evaluating the Effectiveness of Return-to-Work Interventions for Individuals with Work-Related Mental Health Conditions: A Systematic Review and Meta-Analysis. Healthcare. 2023;11(10):1403–1403.
- Mikkelsen M B, Rosholm M. Systematic review and meta-analysis of interventions aimed at enhancing return to work for sick-listed workers with common mental disorders, stress-related disorders, somatoform disorders and personality disorders. Occup Environ Med. 2018;75(9):675–86.
- Brakenridge CL, Smits EJ, Gane EM, Andrews NE, Williams G, Johnston V. Effectiveness of Interventions on Work Outcomes After Road Traffic Crash-Related Musculoskeletal Injuries: A Systematic Review and Meta-analysis. J Occup Rehabil. 2024 Apr 5;
- Wegrzynek P A, Wainwright E, Ravalier J. Return to work interventions for chronic pain: a systematic review. Occup Med Oxf Engl. 2020;70(4):268–77.
- Hult M, Lappalainen K, Saaranen T K, Rasanen K, Vanroelen C, Burdorf A. Health-improving interventions for obtaining employment in unemployed job seekers. Cochrane Database Syst Rev. 2020;1:CD013152.
- de Boer A, Tamminga S, Boschman J, Hoving J. Non‐medical interventions to enhance return to work for people with cancer. Cochrane Database Syst Rev. 2024;(3)
- Cocchiara R A, Sciarra I, D’Egidio V, Sestili C, Mancino M, Backhaus I, et al. Returning to work after breast cancer: A systematic review of reviews. Work Read Mass. 2018;61(3):463–76.
- Lamore K, Dubois T, Rothe U, Leonardi M, Girard I, Manuwald Ulf, et al. Return to Work Interventions for Cancer Survivors: A Systematic Review and a Methodological Critique. Int J Environ Res Public Health. 2019;16(8).
- Cochrane A, Higgins N M, FitzGerald O, Gallagher P, Ashton J, Corcoran O, et al. Early interventions to promote work participation in people with regional musculoskeletal pain: a systematic review and meta-analysis. Clin Rehabil. 2017;31(11):1466–81.
- Lewis T. Proving disability and reasonable adjustments: A worker’s guide to evidence under the Equality Act. 2010.
- GOV.UK [Internet]. 2023 [cited 2025 Jan 17]. Fit note.
Available from: https://www.gov.uk/government/collections/fit-note - Acas [Internet]. 2024 [cited 2025 Jan 17]. What reasonable adjustments are – Reasonable adjustments at work.
Available from: https://www.acas.org.uk/reasonable-adjustments - Grigoroglou C, Munford L, Webb RT, Kapur N, Ashcroft DM, Kontopantelis E. Prevalence of mental illness in primary care and its association with deprivation and social fragmentation at the small-area level in England. Psychol Med. 2019/02/12 ed. 2020;50(2):293–302.
- The King’s Fund [Internet]. [cited 2025 Jan 17]. Mental Health 360 | Inequalities.
Available from: https://www.kingsfund.org.uk/insight-and-analysis/long-reads/mental-health-360-inequalities - Slater D, Venning A, Matthews L, Iles R, Redpath P. Defining work-focused cognitive behavioural therapy (W-CBT) and whether it is effective at facilitating return to work for people experiencing mental health conditions: A systematic review and narrative synthesis. Health Psychol Open. 2023;10(2):20551029231217840.
- Axen I, Bjork B, Elisabeth, Vaez M, Lundin A, Bergstrom G. Interventions for common mental disorders in the occupational health service: a systematic review with a narrative synthesis. Int Arch Occup Environ Health. 2020;93(7):823–38.
- Finnes A, Enebrink P, Ghaderi A, Dahl J, Nager Anna, Ost L-G. Psychological treatments for return to work in individuals on sickness absence due to common mental disorders or musculoskeletal disorders: a systematic review and meta-analysis of randomized-controlled trials. Int Arch Occup Environ Health. 2019;92(3):273–93.
- Brämberg EB, Åhsberg El, Fahlström G, Furberg E, Gornitzki C, Ringborg A, et al. Effects of work-directed interventions on return-to-work in people on sick-leave for to common mental disorders—a systematic review. Int Arch Occup Environ Health. 2024;
- Tingulstad A, Meneses-Echavez J, Evensen Line Holtet, Bjerk M, Berg R C. Effectiveness of work-related interventions for return to work in people on sick leave: a systematic review and meta-analysis of randomized controlled trials. Syst Rev. 2022;11(1).
- Taberna M, Gil Moncayo F, Jané-Salas E, Antonio M, Arribas L, Vilajosana E, et al. The Multidisciplinary Team (MDT) Approach and Quality of Care. Front Oncol. 2020;10.
- Gkiouleka A, Wong G, Sowden S, Kuhn I, Moseley A, Manji S, et al. Reducing health inequalities through general practice: a realist review and action framework. Health Soc Care Deliv Res. 2024;12:07.
- Couturier Y, Lanoue S, Karam M, Guillette M, Hudon C. Social workers coordination in primary healthcare for patients with complex needs: A scoping review. Int J Care Coord. 2023 Mar 1;26(1):5–25.
- Khatri R, Endalamaw A, Erku D, Wolka E, Nigatu F, Zewdie A, et al. Continuity and care coordination of primary health care: a scoping review. BMC Health Serv Res. 2023 Jul 13;23(1):750.
- .Verhoef Joan A C, Bal Marjolijn I, Roelofs Pepijn D D M, Borghouts Jeroen A J, Roebroeck Marij E, Miedema Harald S. Effectiveness and characteristics of interventions to improve work participation in adults with chronic physical conditions: a systematic review. Disabil Rehabil. 2022;44(7):1007–22.
- Blas AJT, Beltran KMB, Martinez PGV, Yao DG. Enabling Work: Occupational Therapy Interventions for Persons with Occupational Injuries and Diseases: A Scoping Review. J Occup Rehabil. 2018;28(2):201–14.
- Nigatu Y T, Liu Y, Uppal M, McKinney S, Rao S, Gillis K, et al. Interventions for enhancing return to work in individuals with a common mental illness: systematic review and meta-analysis of randomized controlled trials. Psychol Med. 2016;46(16):3263–74.
- Kobayashi M, Sezai I, Ishikawa T, Masujima M. Psychological and educational support for cancer patients who return to work: A scoping review. Work Read Mass. 2022;73(1):291–300.
- Butink M, Webers C, Verstappen S, Falzon L, Betteridge N, Wiek D, et al. Non-pharmacological interventions to promote work participation in people with rheumatic and musculoskeletal diseases: a systematic review and meta-analysis from the EULAR taskforce on healthy and sustainable work participation. RMD Open. 2023;9(1):e002903–e002903.
- Guo YJ, Tang J, Li JM, Zhu LL, Xu JS. Exploration of interventions to enhance return-to-work for cancer patients: A scoping review. Clin Rehabil. 2021;35(12):1674–93
- .O’Keefe S, Stanley M, Adam K, Lannin N A. A Systematic Scoping Review of Work Interventions for Hospitalised Adults with an Acquired Neurological Impairment. J Occup Rehabil. 2019;29(3):569–84.
- Coutts E, Cooper K. Return to work for adults following stroke: a scoping review of interventions, factors, barriers, and facilitators. JBI Evid Synth. 2023;21(9):1794–837.
- Dol M, Varatharajan S, Neiterman E, McKnight E, Crouch M, McDonald E, et al. Systematic Review of the Impact on Return to Work of Return-to-Work Coordinators. J Occup Rehabil. 2021;31(4):675–98.
- Bond GR, Al-Abdulmunem M, Marbacher J, Christensen TN, Sveinsdottir V, Drake RE. A Systematic Review and Meta-analysis of IPS Supported Employment for Young Adults with Mental Health Conditions. Adm Policy Ment Health. 2022;
- de Winter L, Couwenbergh C, van Weeghel J, Sanches S, Michon H, Bond GR. Who benefits from individual placement and support? A meta-analysis. Epidemiol Psychiatr Sci. 2022;31:e50.
- Hellstrom L, Pedersen P, Christensen T N, Wallstroem I G, Bojesen A B, Stenager Elsebeth, et al. Vocational Outcomes of the Individual Placement and Support Model in Subgroups of Diagnoses, Substance Abuse, and Forensic Conditions: A Systematic Review and Analysis of Pooled Original Data. J Occup Rehabil. 2021;31(4):699–710.
- Modini M, Tan L, Brinchmann B, Wang M-J, Killackey E, Glozier N, et al. Supported employment for people with severe mental illness: systematic review and meta-analysis of the international evidence. Br J Psychiatry J Ment Sci. 2016;209(1):14–22.
- Suijkerbuijk Y, Schaafsma F, van Mechelen J C, Ojajärvi A, Corbière M, Anema J R. Interventions for obtaining and maintaining employment in adults with severe mental illness, a network meta-analysis. Cochrane Libr. 2017;2017(9).
- Metcalfe J D, Drake R E, Bond G R. Economic, Labor, and Regulatory Moderators of the Effect of Individual Placement and Support Among People With Severe Mental Illness: A Systematic Review and Meta-analysis. Schizophr Bull. 2018;44(1):22–31.
- Wehman P. Supported Employment: What is it? J Vocat Rehabil. 2012 Jan 1;37:139–42.
- Kinoshita Y, Furukawa TA, Kinoshita K, Honyashiki M, Omori IM, Marshall M, et al. Supported employment for adults with severe mental illness. Cochrane Database Syst Rev. 2013;(9).
- Dewa C S, Hoch J S, Loong D, Trojanowski L, Bonato S. Evidence for the Cost-Effectiveness of Return-to-Work Interventions for Mental Illness Related Sickness Absences: A Systematic Literature Review. J Occup Rehabil. 2021;31(1):26–40.