What works: Addressing inequalities in the uptake of cervical screening
There are substantial inequalities in the uptake of cervical screening across socioeconomic and ethnic groups. This brief summarises the evidence on what works to address inequalities in cervical screening and provides recommendations for health practitioners and policymakers.
What works: Addressing inequalities in the uptake of cervical screening[PDF 175kb]
Download documentSummary
Using our Living Evidence Map, we identified 19 research articles examining what works to address inequalities in cervical screening. Interventions fall into four categories:
- Support workers
- Outreach with culturally competent education
- Telephone/mailed reminders, endorsed invitations and scheduled appointment strategies
- Self-sampling
Our 10 evidence-informed recommendations focused on multi-component interventions including support workers for specific disadvantaged communities, culturally competent information, endorsements from a GP and scheduled appointments or self-sampling for those who do not attend. Other key recommendations include disaggregating data, using equity-focused quality improvement, building flexibility into pathways, and creating system flags.
Current challenges
In the UK, cervical screening (also known as a smear test) is offered to women and individuals with a cervix aged 25 to 64 to test for high-risk Human Papillomavirus (HPV), a major cause of cervical cancer, and to check the health of the cervix. There were 753 deaths across England and Wales due to cervical cancer in 2021 (1). Cervical screening has contributed to an 80% reduction in deaths from cervical cancer over the last few decades.
The NHS cervical screening programme (NHSCSP) aims to reduce the number of people who develop cervical cancer, and subsequent mortality. In 2022 NHS England reported that 69.9% of eligible individuals aged 25 to 64 had been adequately screened (2). Latest data from the Office for Health Improvement and Disparities (OHID) for 2021/22 show that the gap in screening coverage between the most and least deprived quintile for women aged 25-49 years is 11% (64.5% in the most deprived and 75.7% in the least deprived, Figure 1) (3). The gap for women aged 50-64 years is 8% (70.2% most deprived and 78.3% least deprived, Figure 1). It is estimated that in England each year 520 cases of cervical cancer are linked with deprivation (4).
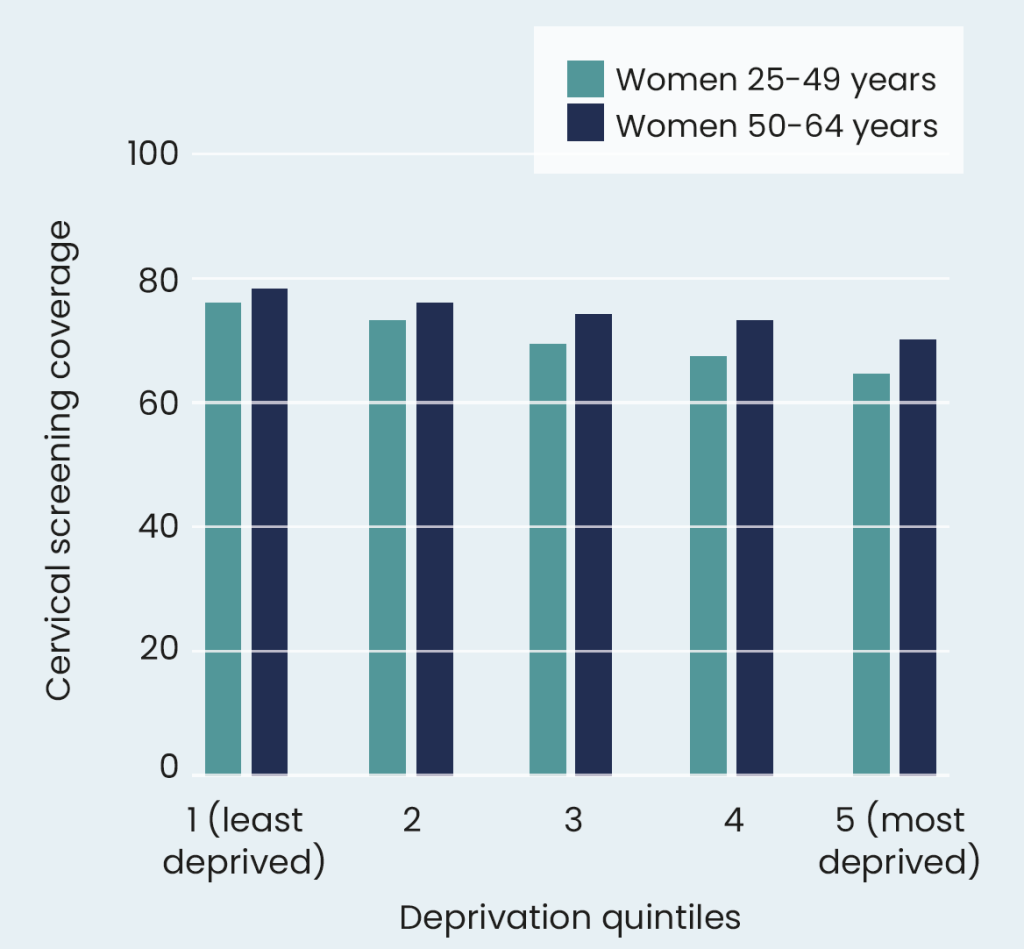
Figure 1: Average percentage of cervical screening coverage of individuals aged 25-64 across deprivation quintiles
The gap in screening coverage between the most and least deprived quintile for women aged 25-49 years was 11% (64.5% in the most deprived and 75.7% in the least deprived). The gap for women aged 50-64 years was 8% (70.2% most deprived and 78.3% least deprived). It is estimated that in England each year 520 cases of cervical cancer are linked with deprivation (4).
Understanding the scale of inequalities across ethnic groups is difficult because of poorly recorded ethnicity data. However, analysis from Hull York Medical School identified inequalities across ethnic groups with Asian women having a 32% lower uptake of cervical screening compared to white women (5). Latest data available from 2017-19 shows that age standardised mortality rates for cervical cancer are higher for black African women (4.9 per 100,000 per year) compared to white women (2.7 per 100,000 per year) (6). This evidence aligns with previously published research identifying socioeconomic (7) and ethnic (8) inequalities in screening uptake.
Summary of evidence
Drawing upon our evidence map, we included 19 research articles examining what works to address inequalities in cervical screening; 16 were either a systematic review, meta-analysis, scoping review or rapid review and three were primary studies.
The research articles identified the following categories of interventions:
- Support workers
- Outreach with culturally competent education
- Telephone/mailed reminders, GP-endorsed invitations, and scheduled appointment strategies
- Self-sampling
Support workers
Ten articles found that support workers were effective in improving cervical screening across socioeconomic and ethnic groups (7,9–17). The majority of interventions were delivered in person at a clinical or community setting. Support workers were often culturally representative of the targeted population group. Two of the systematic reviews (11,14) identified a randomised control trial (RCT) which delivered two workshops (3 hours each) on cervical cancer to women who belong to a minority ethnic group led by support workers. This RCT found a significant difference in screening rates between the intervention and control groups at 6 months (71% compared with 22%) (14). Other approaches which improved uptake included combining support worker home visits with phone support (11). A separate systematic review identified a multi-component approach of support workers offering education, appointment scheduling assistance and reminder/follow-up calls to increase compliance with screening (17).
Outreach with culturally competent education
Complementary to support workers, the impact of outreach education providing culturally competent and relevant information on cervical screening for minority ethnic women has been explored. Eight articles assessed the effectiveness of outreach education for cervical cancer screening for minority ethnic groups (7,9–11,13–15,18).
Research explored informational brochures, visual tools, or a combination. Examples include Atere-Roberts et al.’s (2020) scoping review (13) which included an RCT examining minority ethnic women who had not been screened. They were shown a video with the support of a community worker and were significantly more likely to attend screening than the control group (53% compared with 34%). Chan and So (2015) included a trial focused on women from a minority ethnic group (Samoan) which combined weekly education sessions around cervical cancer with two separate educational booklets. Findings showed that the intervention group were significantly more likely to be screened than the control group (61% compared with 38%) (14).
Telephone/mailed reminders, endorsed invitations, and scheduled appointment strategies
Six papers included telephone/mailed reminders, endorsed invitations, and scheduled appointment strategies that aimed to increase cervical cancer screening (7,11,19–22). A Cochrane review demonstrated that invitations for women who had not attended screening were more successful if they were personalised to include a GP letter or contained a fixed appointment time compared to standard reminders (11). A rapid review identified interventions to improve participant engagement in cancer screening services (19). Of the cervical cancer interventions included in the review, a Dutch national screening programme study found that invitations endorsed by a GP led to a 7.9% higher attendance compared with invitations endorsed by the local health authority, especially for minority ethnic groups.
Self-sampling
Seven papers assessed the efficacy of self-sampling for increasing cervical cancer screening (7,9,21,23–26). Human papillomavirus (HPV) self-sampling is a new method of screening as an alternative to clinician-based screening. HPV self-sampling interventions are delivered by mailed self-test kits or home visits. A systematic review by Rees et al. (2018) highlighted that both methods of delivery showed statistically significant increases in screening across lower socioeconomic groups (7). A separate systematic review/meta-analysis additionally found that providing HPV self-sampling methods was the most effective intervention for improving screening among immigrant women (9). A recent international randomised trial with almost 700 under-screened women from low-income backgrounds compared mailed HPV self-sampling plus support if required with a standard scheduled appointment. Screening uptake was statistically significantly higher in the self-sampling group (72%) than scheduled appointment group (37%) (26).
While self-sampling is currently not included in the national screening programme, there is currently a national study being undertaken to ascertain the effectiveness of self-sampling in the general population of the UK (27).
What works: key recommendations
The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) framework has been adopted to grade the quality of the evidence and support recommendations (28).
| Recommendation | Target audience | GRADE certainty |
| Recommendations from the cervical screening literature |
||
| Based on the cervical screening specific evidence a multi-component approach is needed to address inequalities in cervical screening and should include some or all of the following: | Practices/PCNs/ ICBs | ⊕ ⊕ ⊕ ⊕
High |
|
Practices/PCNs/ ICBs | ⊕ ⊕ ⊕ ⊕
High |
|
Practices/PCNs/ ICBs | ⊕ ⊕ ⊕
Moderate |
|
Practices/PCNs/ ICBs | ⊕ ⊕ ⊕
Moderate |
|
ICBs/ National | ⊕ ⊕
Low |
|
Practices/PCNs/ ICBs | ⊕ ⊕ ⊕
Moderate |
| Recommendations from transferrable equity-focused literature | ||
| Data disaggregated by socioeconomic group and ethnicity is needed to understand and tracking inequalities in uptake of cervical screening. | Practices/PCNs/ ICBs | ⊕ ⊕ ⊕
Moderate |
| Practices should consider how to increase their flexibility in their approach to cervical screening, such as opening hours, location, offering double appointments or combining with other GP surgery visits (evidence from EQUALISE study) (29). | Practices/PCNs | ⊕ ⊕
Low |
| Practices and primary care networks should use equity-focused quality improvement principles to improve overall cervical screening coverage in addition to addressing inequalities (see our complementary guide on How to undertake Equity-Focused Quality Improvement). | Practices/PCNs/ ICBs | ⊕ ⊕
Low |
| Practices should consider systematic flagging of patient records to identify those who may be vulnerable to inequalities in cancer screening (see evidence from FAIRSTEPS) (30). | Practices | ⊕
Very Low |
Case study
Health professionals in Norfolk and Suffolk have implemented a targeted cervical screening programme using the Eclipse/NHS Pathways data to identify patients who were eligible for cervical screening but overdue. Patients identified were reviewed by practices and received targeted letters and phone calls. Findings from the interventions show that an additional 12-14% of eligible patients attended cervical screening appointment following the intervention; 459 people who would not have otherwise been screened. More details can be found here.
Useful resources
How this brief was produced
What is the Living Evidence Map on What Works to address health inequalities in primary care?
Using AI-powered software called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles that examine interventions to address inequalities. The evidence map contains systematic reviews and umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
References
- Nomis – Official Census and Labour Market Statistics [Internet]. 2021 [cited 2023 Oct 20]. Available from: https://www.nomisweb.co.uk/
- NHS Digital [Internet]. 2022 [cited 2023 Oct 10]. Cervical Screening Programme, England – 2021-2022 [NS]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/cervical-screening-annual/england-2021-2022
- Cancer Services – Data – OHID [Internet]. 2023 [cited 2023 Oct 17]. Available from: https://fingertips.phe.org.uk/profile/cancerservices/data#page/4/gid/1938133365/pat/159/par/K02000001/ati/15/are/E92000001/iid/93725/age/299/sex/4/cat/-1/ctp/-1/yrr/1/cid/4/tbm/1/page-options/tre-do-1
- Cancer Research UK [Internet]. 2015 [cited 2023 Oct 11]. Cervical cancer statistics. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer
- Chilekwa D, Cairns J, Pitel L. A cross-sectional analysis of ethnic inequalities in cervical screening uptake in the uk using understanding society. 2022. Available from: https://ukdataservice.ac.uk/app/uploads/chilekwa.pdf
- Office for National Statistics [Internet]. 2023 [cited 2023 Oct 20]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/adhocs/15495agestandardisedmortalityratesforuterineandcervicalcancerbyethnicgroupfemalesaged10andabovedeathsregisteredinenglandandwales2012and2019
- Rees I, Jones D, Chen H, Macleod U. Interventions to improve the uptake of cervical cancer screening among lower socioeconomic groups: A systematic review. Preventive Medicine. 2018 Jun 1;111:323–35.
- Moser K, Patnick J, Beral V. Inequalities in reported use of breast and cervical screening in Great Britain: analysis of cross sectional survey data. BMJ. 2009 Jun 16;338:b2025.
- Alam Z, Cairns JM, Scott M, Dean JA, Janda M. Interventions to increase cervical screening uptake among immigrant women: A systematic review and meta-analysis. PLoS One. 2023 Jun 2;18(6):e0281976.
- Kelly C, Pericleous M, Hendy J, De Lusignan S, Ahmed A, Vandrevala T, et al. Interventions to improve the uptake of screening across a range of conditions in Ethnic Minority Groups: a systematic review. Int J Clin Pract. 2018 Aug;72(8):e13202.
- Staley H, Shiraz A, Shreeve N, Bryant A, Martin-Hirsch PP, Gajjar K. Interventions targeted at women to encourage the uptake of cervical screening. Cochrane Database of Systematic Reviews [Internet]. 2021 [cited 2023 Oct 23];(9). Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD002834.pub3/full
- Korn AR, Walsh-Bailey C, Correa-Mendez M, DelNero P, Pilar M, Sandler B, et al. Social determinants of health and US cancer screening interventions: A systematic review. CA: A Cancer Journal for Clinicians. 2023;73(5):461–79.
- Atere-Roberts J, Smith JL, Hall IJ. Interventions to increase breast and cervical cancer screening uptake among rural women: a scoping review. Cancer Causes Control. 2020 Nov 1;31(11):965–77.
- Chan DNS, So WKW. A systematic review of randomised controlled trials examining the effectiveness of breast and cervical cancer screening interventions for ethnic minority women. European Journal of Oncology Nursing. 2015 Oct 1;19(5):536–53.
- Escribà-Agüir V, Rodríguez-Gómez M, Ruiz-Pérez I. Effectiveness of patient-targeted interventions to promote cancer screening among ethnic minorities: A systematic review. Cancer Epidemiology. 2016 Oct 1;44:22–39.
- Fuzzell LN, Perkins RB, Christy SM, Lake PW, Vadaparampil ST. Cervical cancer screening in the United States: Challenges and potential solutions for underscreened groups. Preventive Medicine. 2021 Mar 1;144:106400.
- Mistry S K, Harris E, Harris M. Community Health Workers as Healthcare Navigators in Primary Care Chronic Disease Management: a Systematic Review. Journal of General Internal Medicine. 2021;5:05.
- Han HR, Kim J, Lee JE, Hedlin HK, Song H, Song Y, et al. Interventions that increase use of Pap tests among ethnic minority women: a meta-analysis. Psychooncology. 2011 Apr;20(4):341–51.
- Duffy SW, Myles JP, Maroni R, Mohammad A. Rapid review of evaluation of interventions to improve participation in cancer screening services. J Med Screen. 2017 Sep 1;24(3):127–45.
- Spadea T, Bellini S, Kunst A, Stirbu I, Costa G. The impact of interventions to improve attendance in female cancer screening among lower socioeconomic groups: a review. Preventive Medicine. 2010;50(4):159–64.
- Sun L, Patel S, Fiorina C, Glass A, Rochaix L, Bardou M, et al. A systematic review of the cost-effectiveness of interventions to increase cervical cancer screening among underserved women in Europe. Eur J Health Econ [Internet]. 2023 Sep 20 [cited 2023 Oct 23]; Available from: https://doi.org/10.1007/s10198-023-01627-1
- Firmino-Machado J, Varela S, Mendes R, Moreira A, Lunet N, SCAN-Cervical Cancer collaborators. Stepwise strategy to improve cervical cancer screening adherence (SCAN-Cervical Cancer) – Automated text messages, phone calls and reminders: Population based randomized controlled trial. Preventative Medicine. 2018 Sep;114:123–33.
- Yeh PT, Kennedy CE, Vuyst H de, Narasimhan M. Self-sampling for human papillomavirus (HPV) testing: a systematic review and meta-analysis. BMJ Global Health. 2019 May 1;4(3):e001351.
- Di Gennaro G, Licata F, Trovato A, Bianco A. Does self-sampling for human papilloma virus testing have the potential to increase cervical cancer screening? An updated meta-analysis of observational studies and randomized clinical trials. Frontiers in Public Health [Internet]. 2022 [cited 2023 Oct 23];10. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1003461
- Pretsch PK, Spees LP, Brewer NT, Hudgens MG, Sanusi B, Rohner E, et al. Effect of HPV self-collection kits on cervical cancer screening uptake among under-screened women from low-income US backgrounds (MBMT-3): a phase 3, open-label, randomised controlled trial. The Lancet Public Health. 2023 Jun 1;8(6):e411–21.
- Kobetz E, Seay J, Koru-Sengul T, Bispo JB, Trevil D, Gonzalez M, et al. A randomized trial of mailed HPV self-sampling for cervical cancer screening among ethnic minority women in South Florida. Cancer Causes Control. 2018 Sep 1;29(9):793–801.
- HPValidate cervical screening self-sampling study nears completion – UK National Screening Committee [Internet]. 2023 [cited 2023 Oct 31]. Available from: https://nationalscreening.blog.gov.uk/2023/06/21/hpvalidate-cervical-screening-self-sampling-study-nears-completion/
- What is GRADE? BMJ Best Practice [Internet]. 2023 [cited 2023 Oct 12]. Available from: https://bestpractice.bmj.com/info/toolkit/learn-ebm/what-is-grade/
- Gkiouleka A, Wong G, Sowden S, Bambra C, Siersbaek R, Manji S, et al. Reducing health inequalities through general practice. The Lancet Public Health. 2023 Jun 1;8(6):e463–72.
- Jackson B, Ariss S, Burton C, Coster J, Reynolds J, Lawy T, et al. The FAIRSTEPS Study: Framework to Address Inequities in pRimary care using STakEholder PerspectiveS – short report and user guidance [Internet]. The University of Sheffield; 2023 Feb [cited 2023 Nov 21]. Available from: https://orda.shef.ac.uk/articles/report/The_FAIRSTEPS_Study_Framework_to_Address_Inequities_in_pRimary_care_using_STakEholder_PerspectiveS_-_short_report_and_user_guidance/22040813/1
Suggested citation
Torres O, Dehn Lunn A, Ford J. ‘What works – Addressing inequalities in the uptake of cervical screening’, Evidence Brief, Health Equity Evidence Centre, 2024
