GP Contract 2024/25: More Money, Same Problems?

The additional £899m investment in general practice is a welcome step forward, and its positive impact should not be underestimated. The increase in global sum funding is a strong move, reinforcing the importance of capitation as a foundation for an equitable funding system. However, the Carr-Hill formula, which underpins funding allocation, reflects activity rather than need. The additional investment within the current funding streams shows that simply increasing investment without contract reform risks reinforcing existing funding inequalities.
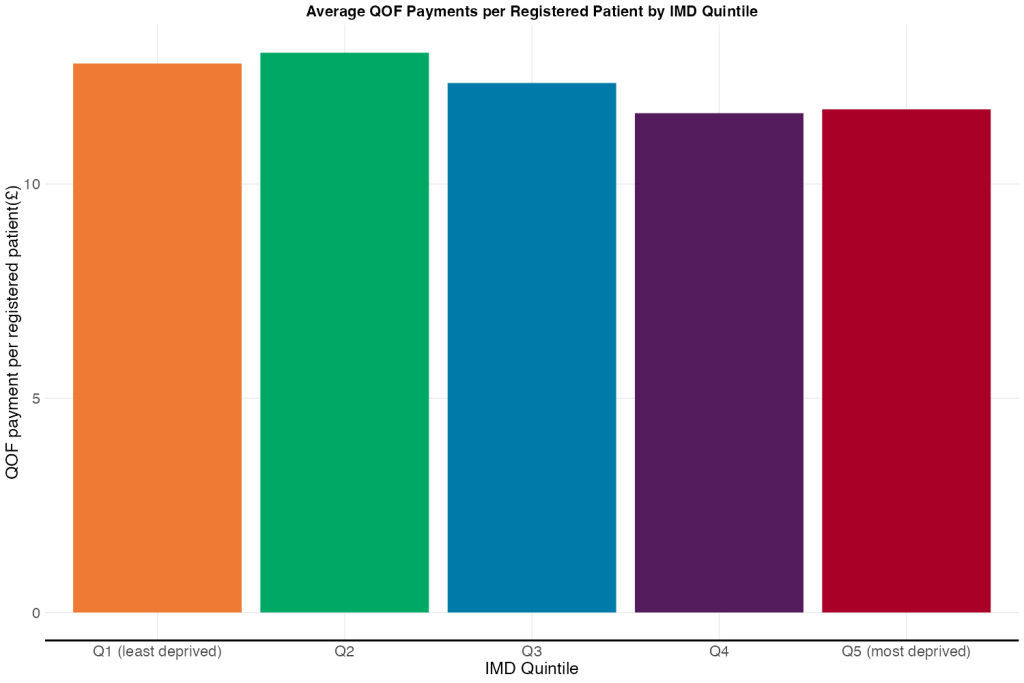
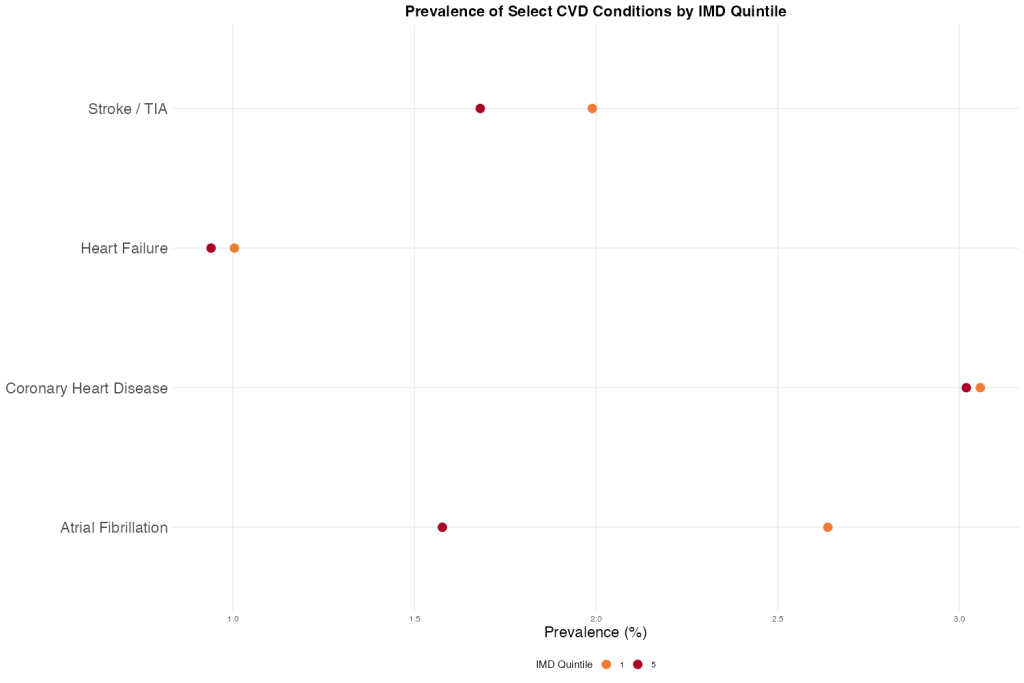
QOF Adjustments
In the most recent data, practices in the least deprived areas received £12.80 in QOF payments per patient, compared to £11.70 in the most deprived. The redistribution of QOF funding to focus on cardiovascular disease (CVD) is a welcome step, given that CVD is one of the biggest drivers of inequalities in life expectancy. However, recent data show that recorded prevalence of CVD is slightly higher in more affluent areas, possibly because wealthier areas tend to have older populations. Since one of the elements that QOF payments are adjusted based on is recorded prevalence, this may mean that practices in wealthier areas continue to receive more funding—potentially limiting the equity impact of the changes.
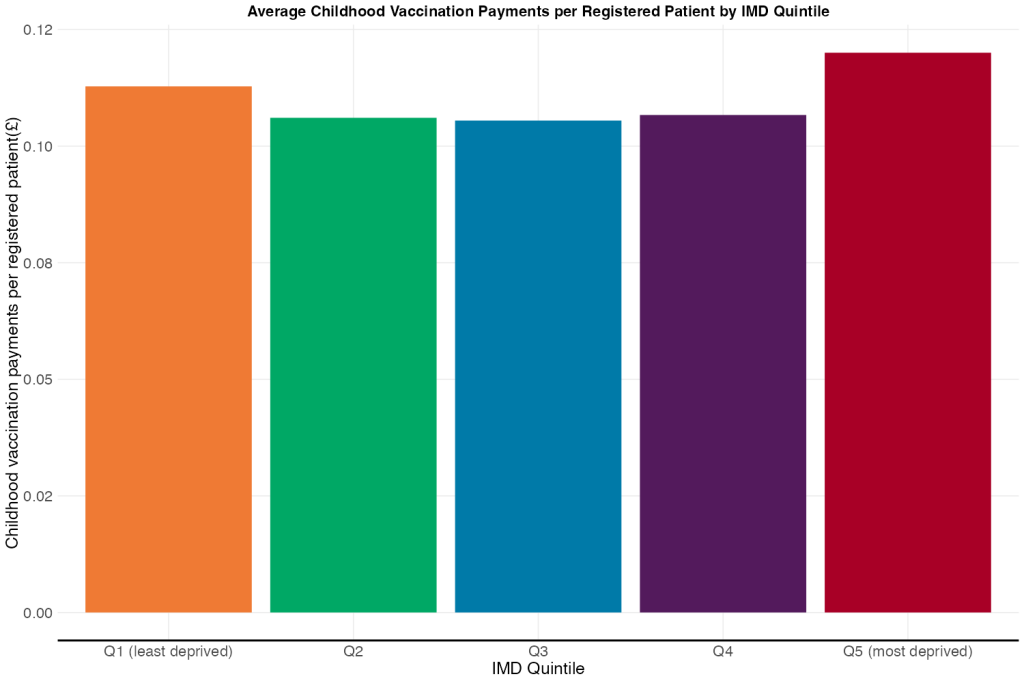
Vaccination Payments
Increasing Item of Service (IoS) payments for childhood vaccinations may slightly reduce funding disparities, as more deprived areas tend to have younger populations and deliver more childhood vaccinations. However, childhood vaccination payments make up a very small proportion of total funding—just ~£0.11 per patient compared to over £12 from QOF payments alone—so the effect on overall equity is minimal. Moreover, the payment uplift does not fully account for the greater effort required to vaccinate underserved populations, where hesitancy tends to be higher and outreach more resource-intensive.
ARRS Changes
The increased flexibility in Additional Roles Reimbursement Scheme (ARRS) funding is welcome, but its impact on tackling workforce shortages in deprived areas remains uncertain. Historically, practices in more affluent areas have found it easier to recruit and retain GPs, although there are now more GPs looking for work than ever before. To ensure equity, PCN and ARRS funding should be allocated using a weighted formula that prioritises areas with higher deprivation and greater workforce need.
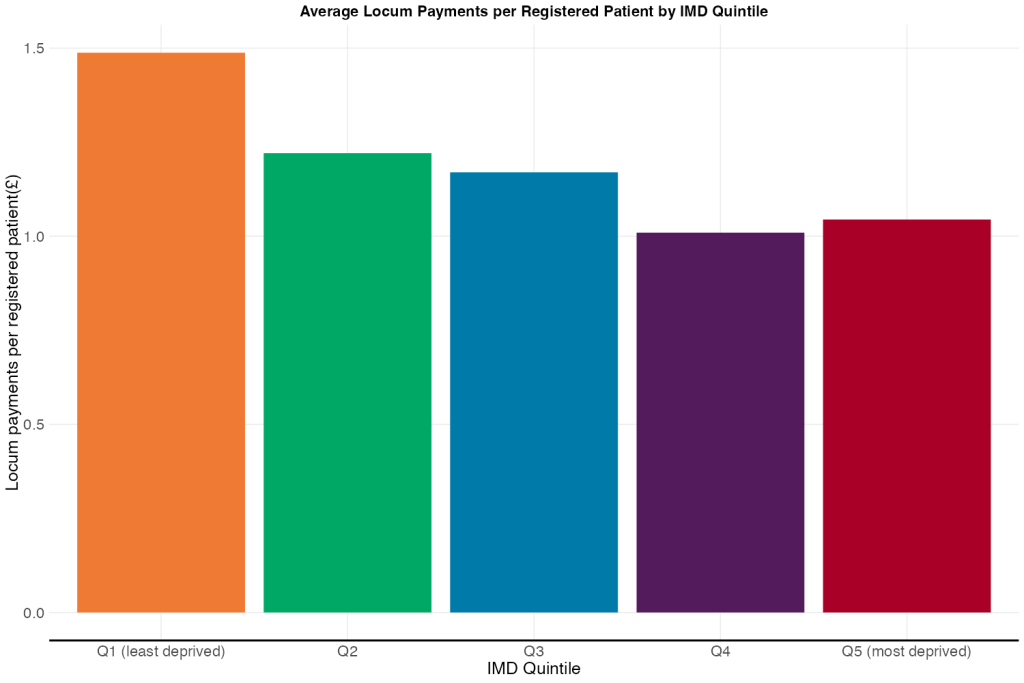
Locum Reimbursement
While increasing locum reimbursement rates is a positive change, the existing gap in locum pay between wealthier and more deprived areas means this change is unlikely to reduce funding inequalities. Practices in affluent areas already have higher locum rates, so they are likely to benefit more than those struggling with recruitment.
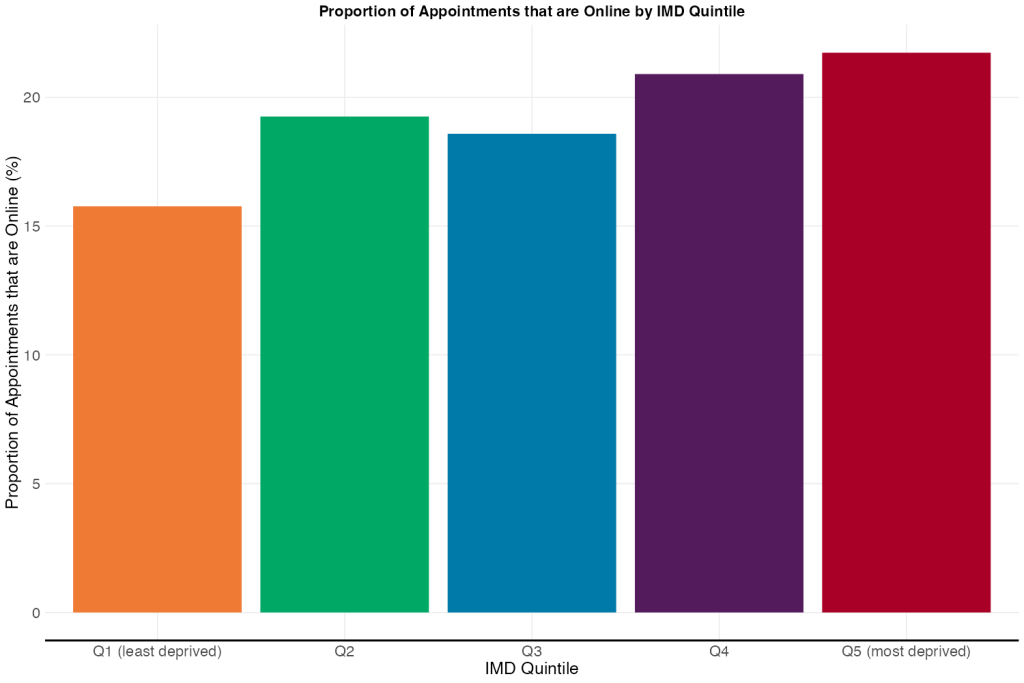
Digital Access
The mandate to keep online consultation tools open throughout core hours is a positive step towards improving access, particularly for those comfortable with digital healthcare. However, there is no additional support for practices to help patients with low digital literacy, which could lead to further exclusion of vulnerable groups. A more proactive approach, including funding for digital inclusion initiatives, should be considered to ensure online access benefits all patients equally.
Capacity and Access Improvement Payments
The continuation of Capacity and Access Improvement (CAIP) payments is an encouraging move, particularly if they are used to target resources towards the most disadvantaged groups. To maximise impact, practices must be supported in implementing population health approaches, ensuring that funding is directed towards patients with the highest unmet needs.
GP Contract Reform
While the new contract introduces important investments, funding allocation remains constrained by legacy formulas that do not adequately reflect need. To genuinely reduce inequalities, wider funding reform that considers all elements of GP funding (including the Carr-Hill formula) is required.
