Do practices with more funding employ more staff and achieve better patient satisfaction?

Previous research has shown an association between funding and patient experience; practices receiving less funding have lower levels of patient satisfaction. Our work explores how funding, workforce and patient experience are related.
In short, the answer is yes – more funding equals more staff and better patient satisfaction – but the effect is small, and the increase in patient satisfaction is only partly explained by the increased workforce.
Previous research has shown an association between funding and patient experience; practices receiving less funding have lower levels of patient satisfaction. Our work explores how funding, workforce and patient experience are related.
Where we are now with funding, workforce and patient satisfaction?
Practices received on average £152 per patient funding from the NHS in 2019. Most of this comes through capitation, a payment per weighted patient using a formula widely known as the Carr-Hill formula. It has been criticised for being outdated and poorly reflective of socioeconomic need. Practices serving more deprived populations receive around 7% less funding per weighted patient than those serving more affluent neighbourhoods.
On average practices employed 5.6 full-time equivalent GPs. The number of fully qualified full-time equivalent GPs between 2015 and 2024 has been steadily decreasing despite increasing patient complexity and demand. Moreover, there are inequalities with more GPs in more affluent areas.
Patient satisfaction has been decreasing since 2015, and in 2023 it dropped to a record low of 71.3%. In 2019, 83% of patients rated practices as good or very good for overall experience, 69% good or very good for access, 49% good or very good for continuity and 95% good or very good for trust. But inequalities exist; practices in more deprived areas have consistently lower patient satisfaction.
What did we do?
We examined 6,139 practices (about 90% of all practices in England) focusing on the period just before the pandemic. We linked data from publicly available datasets: ‘NHS Payments to General Practice’, ‘General Practice Workforce’, ‘GP Patient Survey Data’ and ‘National General Practice Profiles’ by practice code, and undertook a mediation analysis to investigate how much of the relationship between funding and patient satisfaction can be explained by an increase in GP workforce.
What did we find?
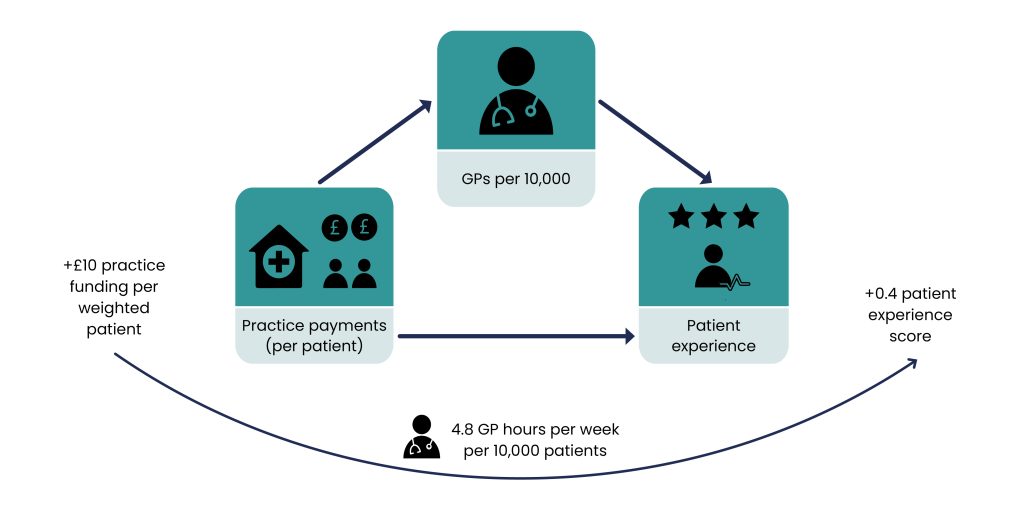
We found that funding, workforce and patient satisfaction were linked by a causal chain such that increased practice payments were associated with increased patient experience, and this was partly explained by increased GPs. An increase of £10 practice funding per registered patient resulted in an increase in patient satisfaction of 0.4%, which is partially explained by the funding causing an increase in the workforce by 4.8 GP hours per 10,000 patients.
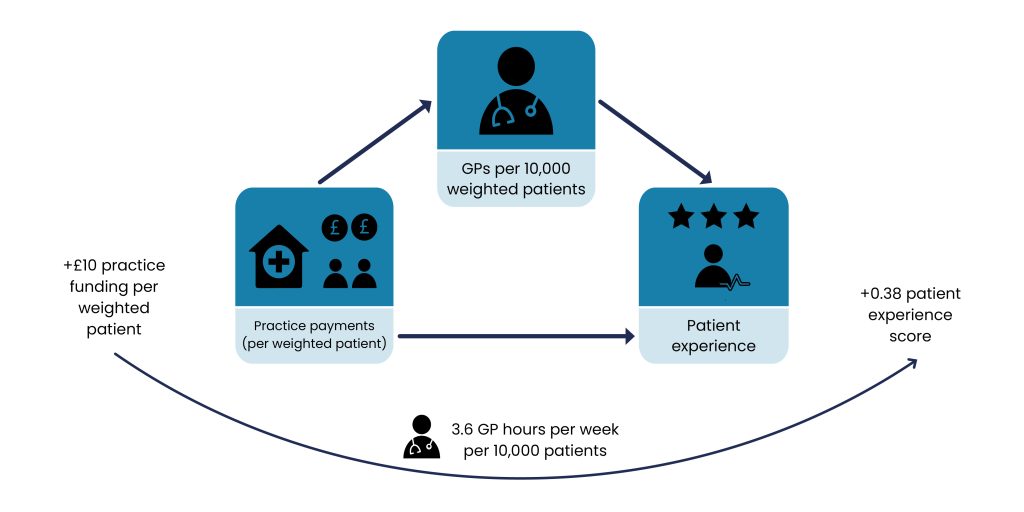
Given that there is increased workload associated with greater health needs, we also analysed this mediation effect considering needs-adjusted registered patients (weighted patients). We found a similar effect: that GP supply mediated the relationship between practice funding and patient experience.
Why is this important?
There have been repeated calls to increase funding to general practice. Our findings suggest that increasing funding will increase workforce and patient satisfaction, but not as much as policymakers and practitioners may think – more money is only part of the answer. To improve patient satisfaction, increased funding needs to come hand-in-hand with service transformation to improve timely access, quality and outcomes.
It is also important to note that given that deprived practices have worse patient satisfaction, GPs per capita and practice funding, we expect that policy reforms could have an impact on health inequalities.
How can I find out more?
If you want to read more, please see our recently published paper: https://bmjopen.bmj.com/content/14/2/e072498#ref-2
