Applying a missingness lens to healthcare – missed appointments letters – tear up and start again!

In this guest blog, Professor Andrea Williamson reflects on her previous research into repeated missed healthcare appointments, which links high non-attendance to poorer health outcomes and social disadvantage. Building on this work, she introduces a new approach to appointment letters aimed at better supporting patients and improving engagement with services.
For decades there has been a focus on missed appointments; however, this has primarily centred on the impact of missed appointments at the service level such as cost to the NHS of missed appointments [1] rather than at the patient level, and makes no distinction between one off ‘situational’ missed appointments and more enduring patterns [2]. Our previous large-scale, award-winning research investigated patterns of missed appointments at the patient level in the general population, using over half a million Scottish general practice (GP) patient records [3].
We found that a high rate of missed GP appointments (an average of more than two per year) predicted very high premature death rates. These patients were more likely to have multi-morbidity (two or more co-existing long-term health issues), especially mental health conditions [4], and to experience high socio-economic disadvantage and other challenging social factors [3][5]. They also experienced high treatment burden – the ongoing work needed to manage their health – and were at greater risk of missing outpatient hospital appointments [6].
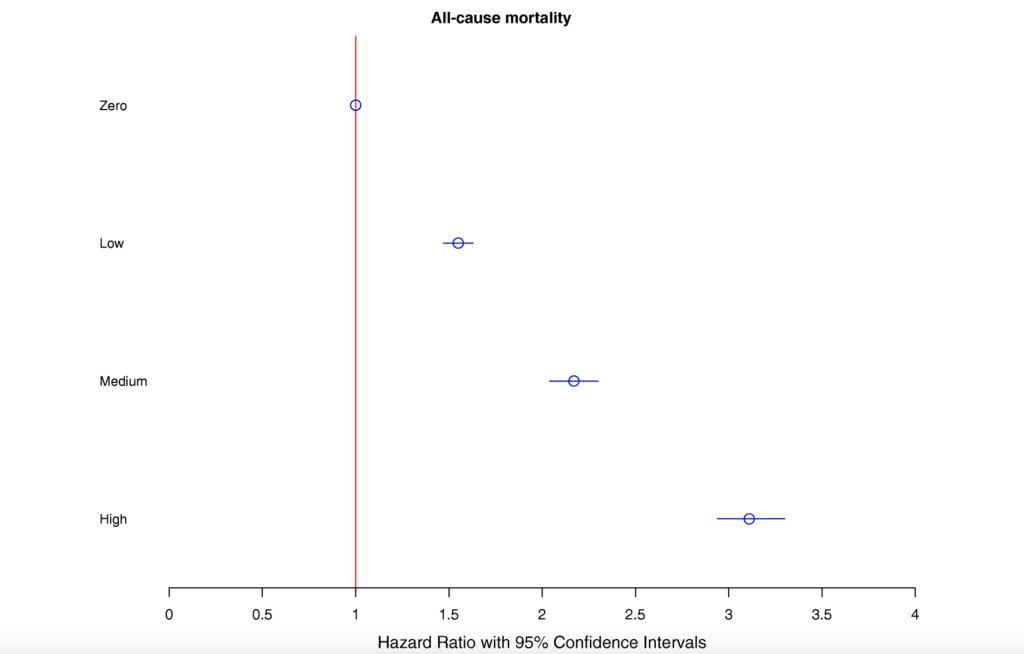
Figure 1 shows the risk of dying for zero, low, medium and high number of missed appointment groupings [4]. If this stark difference in associated outcomes were for a health condition rather than health service utilisation patterns, there would be outrage.
The existing research was limited in explaining why people might miss healthcare appointments and what could be done to address this. It tended to frame the issue as being the patients’ fault and a problem for services. It was also seen as dealing with single issues, like forgetfulness, and thus often proposed ‘one size fits all’ and overly simplistic solutions [2].
Understanding the causes of missingness
We define missingness as the ‘repeated tendency not to take up offers of care such that it has a negative impact on the person and their life chances’ [7].
Using realist methods in our new research, we have developed a ‘programme theory’ about the causes of missingness as shown in the short film below [2].
The Scottish Government’s Primary Care Directorate took the earlier epidemiological research findings seriously, and addressing missingness became part of the focus of funding awarded to around 70 Deep End GP practices in Glasgow over the past two years. In tandem with our research, these practices have been grappling with what practical changes are needed. Dr Elspeth Strang and Dr Peter Cawston, the GPs who lead this work on behalf of the Scottish Government, decided that previous missed appointment letters needed to be torn up and rewritten.
This is the template letter we have produced, and we are hopeful this will influence how practices write them in the future.
For more information about the research, outputs and ongoing activity visit the project webpage
References
- England N. Missed GP appointments costing NHS millions. UK: NHS England; 2019.
- Lindsay C, Baruffati D, Mackenzie M, Ellis DA, Major M, O’Donnell CA, et al. Understanding the causes of missingness in primary care: a realist review. BMC Medicine. 2024;22(1):235.
- Williamson AE, Ellis DA, Wilson P, McQueenie R, McConnachie A. Understanding repeated non-attendance in health services: a pilot analysis of administrative data and full study protocol for a national retrospective cohort. BMJ Open. 2017;7.
- McQueenie R, Ellis DA, McConnachie A, Wilson P, Williamson AE. Morbidity, mortality and missed appointments in healthcare: a national retrospective data linkage study. BMC Medicine. 2019;17(1):2.
- Williamson AE, McQueenie R, Ellis DA, McConnachie A, Wilson P. General practice recording of adverse childhood experiences: a retrospective cohort study of GP records. BJGP Open. 2020:bjgpopen20X101011.
- Williamson AE, McQueenie R, Ellis DA, McConnachie A, Wilson P. ‘Missingness’ in health care: Associations between hospital utilization and missed appointments in general practice. A retrospective cohort study. PLOS ONE. 2021;16(6):e0253163.
- Lindsay C, Baruffati D, Mackenzie M, Ellis D, Major M, O’Donnell K, et al. A realist review of the causes of, and current interventions to address missingness in health care. NIHR Open Research. 2023;3(33).
About the author: Andrea Williamson is a Professor of General Practice and Inclusion Health, combining teaching, research and clinical practice. She teaches and trains about the social determinants of health, Inclusion Health practice and trauma-informed care. She leads on research about “missingness” in healthcare and is involved in wider research and policy work to improve care for people experiencing severe and multiple disadvantage. Andrea is also a founding member of GPs at the Deep End Scotland.