Improving mental health care for Black men

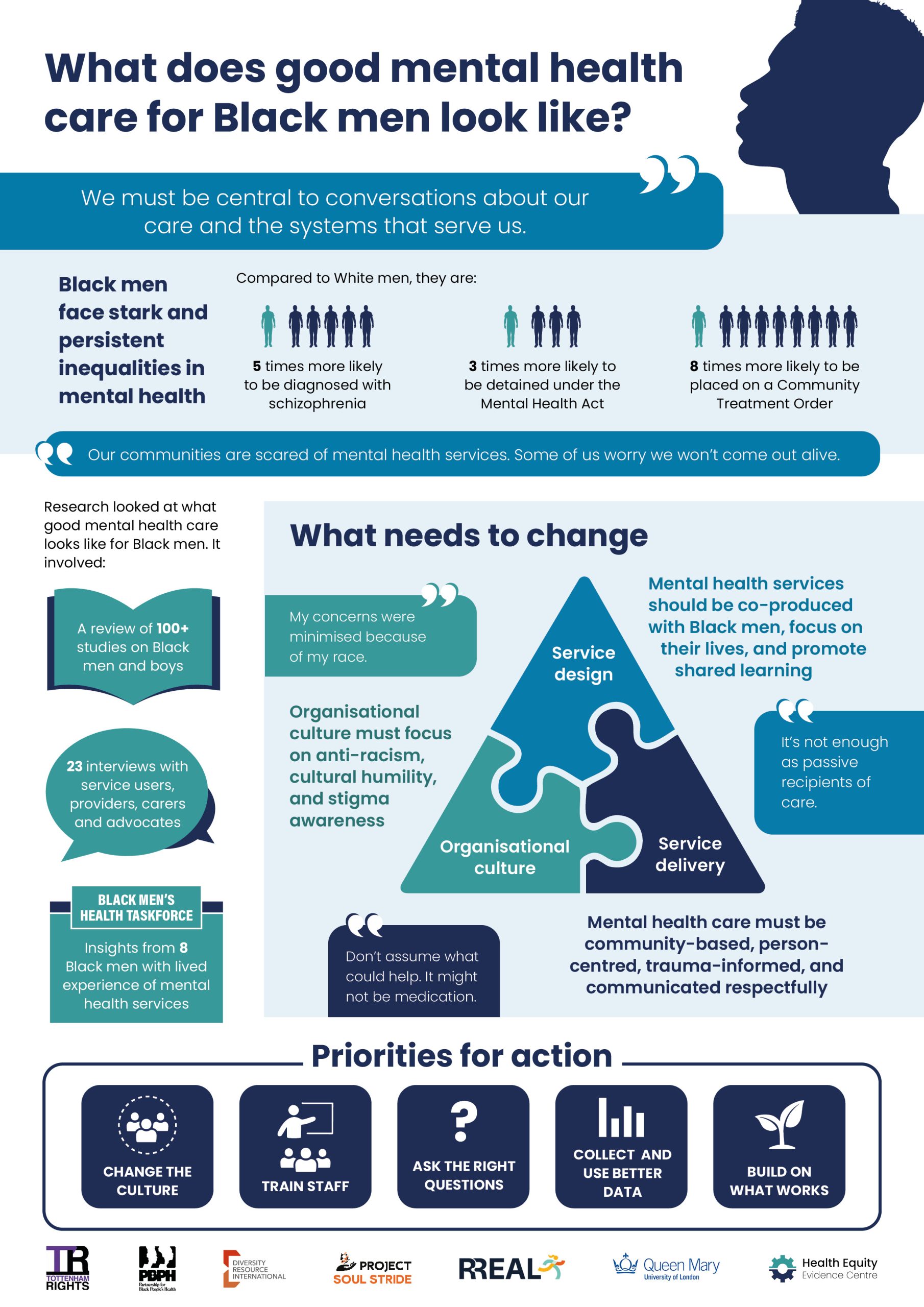
Black men face stark inequalities in mental health — from higher rates of diagnosis and detention to poorer access and outcomes. This brief highlights what needs to change to make care safer, fairer and more effective. Based on evidence and lived experience, it identifies changes in organisational culture, mental health service design and delivery, and sets out five clear priorities for action.
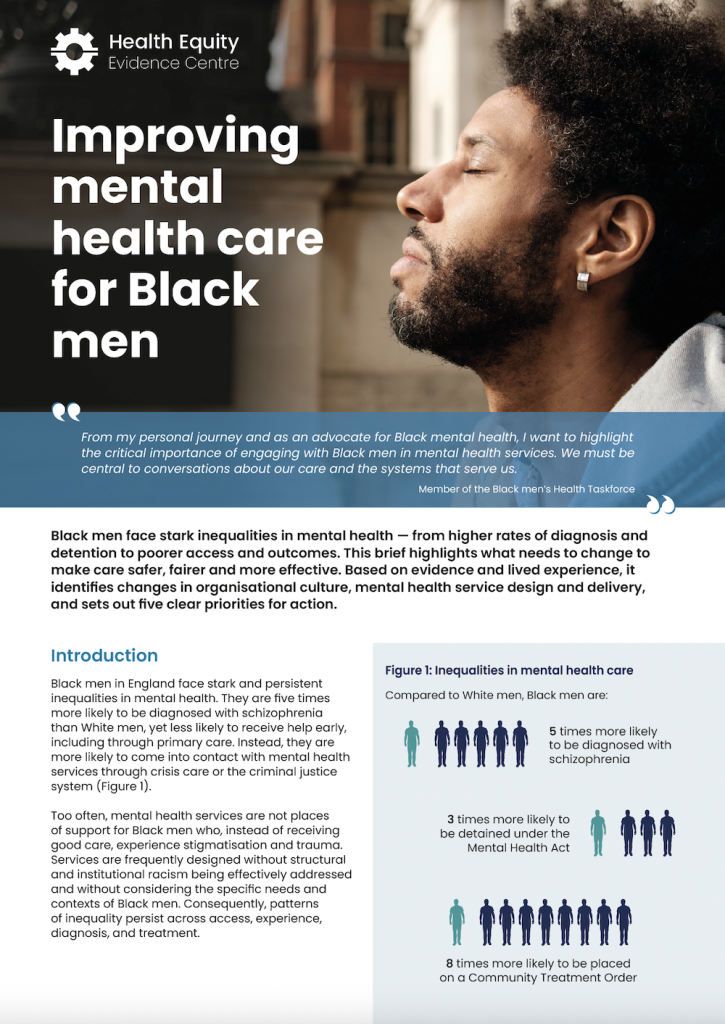
Black men in England face stark and persistent inequalities in mental health. They are five times more likely to be diagnosed with schizophrenia than White men, yet less likely to receive help early, including through primary care. Instead, they are more likely to come into contact with mental health services through crisis care or the criminal justice system.
Too often, mental health services are not places of support for Black men who, instead of receiving good care, experience stigmatisation and trauma. Services are frequently designed without structural and institutional racism being effectively addressed and without considering the specific needs and contexts of Black men. Consequently, patterns of inequality persist across access, experience, diagnosis, and treatment.
This brief highlights what needs to change to make care safer, fairer and more effective. It is based on an independent review of the literature and interviews with service users, providers, carers and advocates, commissioned by the Care Quality Commission and supported by the Black Men’s Health Taskforce.