Data analysis of structural inequalities in primary care.
Which ICB’s have the greatest need for primary care?
Different populations have different needs for primary care. The NHS measures healthcare need by accounting for the populations’ demographic characteristics and overall health status to produce a ‘weighted’ population count (1).
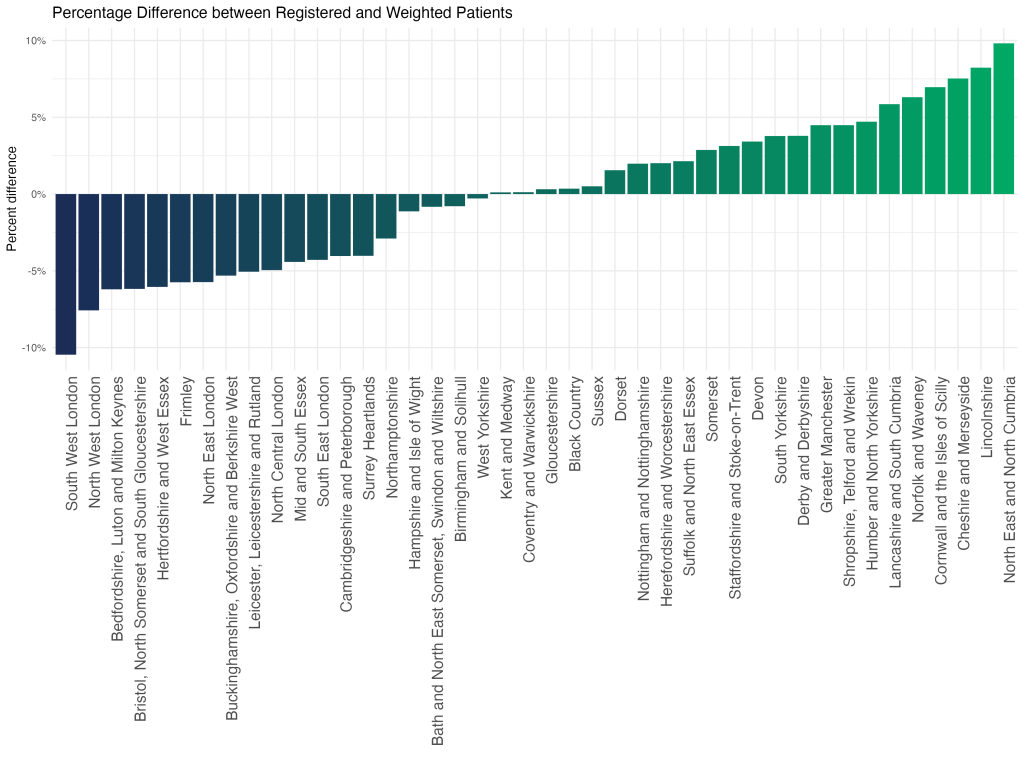
This chart demonstrates that the ICBs with the greatest healthcare need relative to population size are North East and North Cumbria, Lincolnshire, and Cheshire and Merseyside.
This pattern reflects a combination of demographics, such as the number of older people, socio-economic disadvantage, such as the level of poverty, and the health of the population.
Which ICBs have the highest concentration of GP surgeries in socio-economically disadvantaged areas?
The NHS has developed an approach – Core20PLUS5 – to target the most socio-economically disadvantaged 20% of the national population, as identified by the Index of Multiple Deprivation (IMD). Levels of deprivation vary between ICBs; to understand the distribution of GP surgeries across the socio-economic gradient we have divided practices into quintiles from most to least deprived, based on the IMD of the populations served.
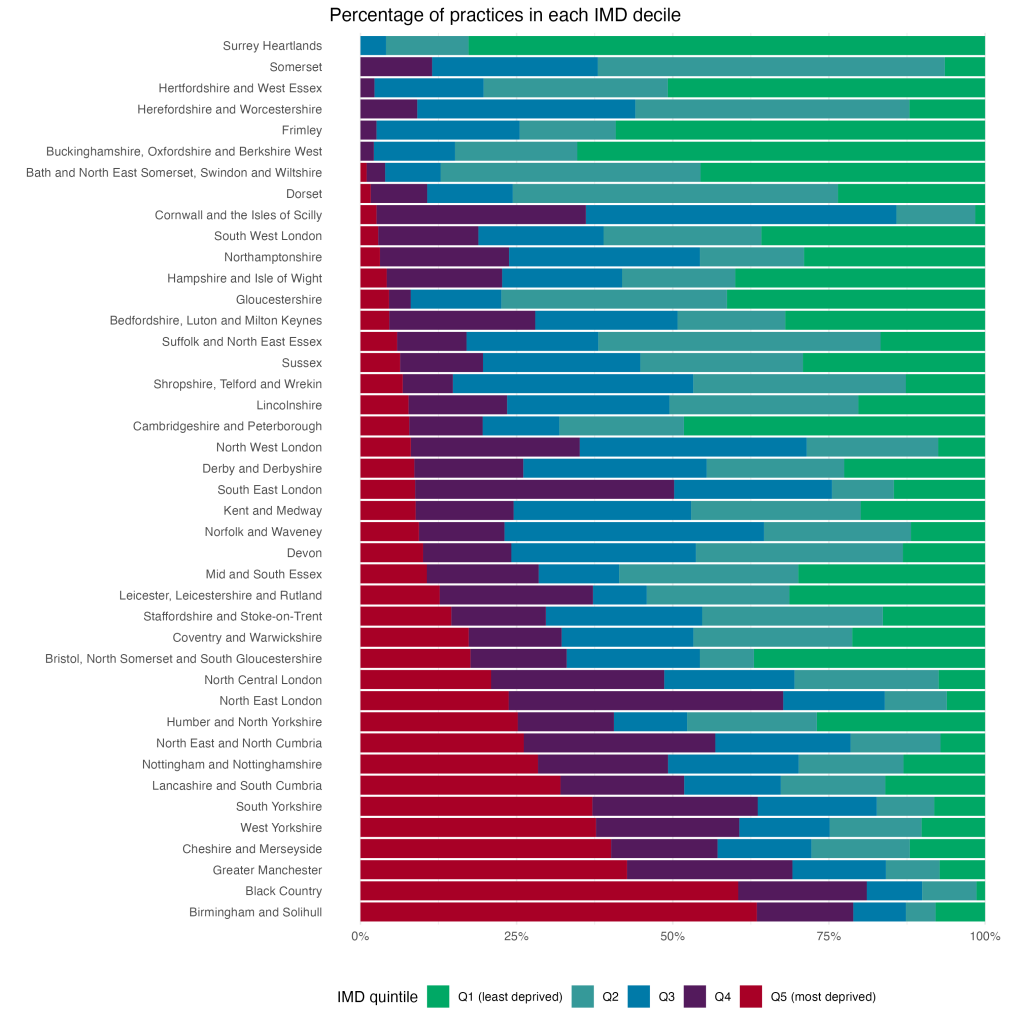
This chart illustrates that over 60% over practices in Birmingham & Solihull and the Black Country serve populations that are predominantly in the most deprived quintile of the national population. Whereas there are no practices in the Surrey Heartlands or Somerset which are in the lowest deprivation quintile based on an average of the population they serve.
This does not mean that there are not pockets of poverty and disadvantage in Surrey Heartlands or Somerset, rather when all the patients in each practice are combined the average is not in the lowest quintile.
How does NHS funding to GP surgeries vary across socio-economic groups?
In order to ensure equitable primary care, practices serving populations with higher healthcare need should receive commensurately higher funding. Here we plot how funding has changed over time by socio-economic group across England.
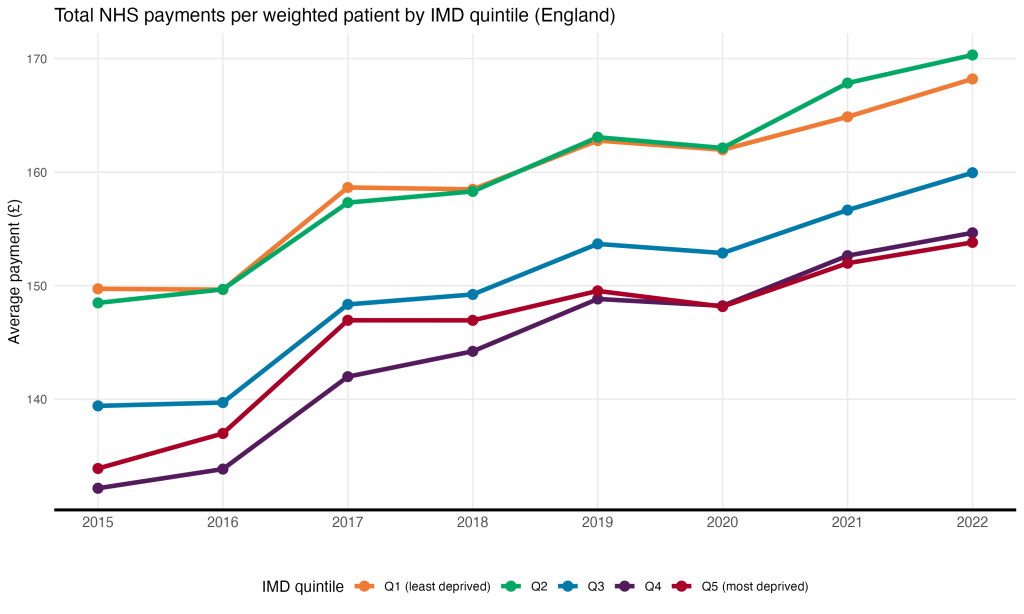
Practices serving the most deprived 20% of the population received £14 less in NHS payments per weighted patient in 2022 than their counterparts serving patients in the top quintile; in 2015, the difference was £16.
What drives the inequalities in NHS funding across socio-economic groups?
Practices receive income based on their population (capitation payment) and for providing additional services or meeting quality standards. The largest proportion, the Global Sum, is allocated based on the number of patients and their estimated health need.
Even though Global Sum payments are supposed to account for healthcare need, the practices serving the most deprived quintile (Q5) still receive fewer payments from the NHS than practices serving the least deprived quintile (Q1). Therefore, Q1 must be receiving relatively more payments in the other categories.
Here we divide payments in each quintile into several different categories (2) and determine the proportion of total payments of each category in each quintile in 2022.
Payments by type by IMD quintile, England (2022)
In relative terms, prescribing payments constitute 13% of Q1’s payments, versus only 2% of payments to Q5. As such, the socio-economic gradient in payments is largely driven by differences in prescribing payments.
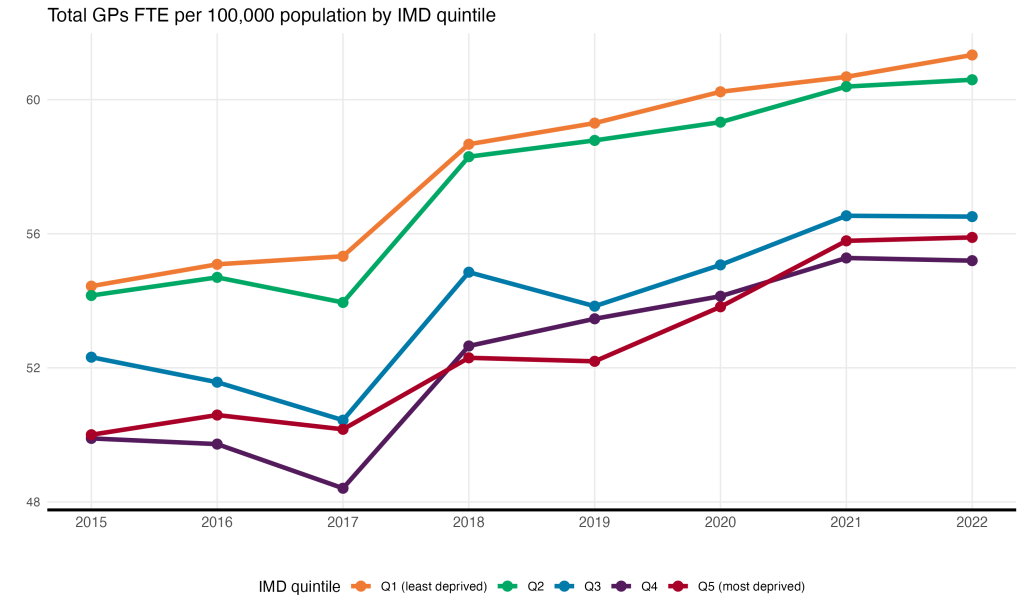
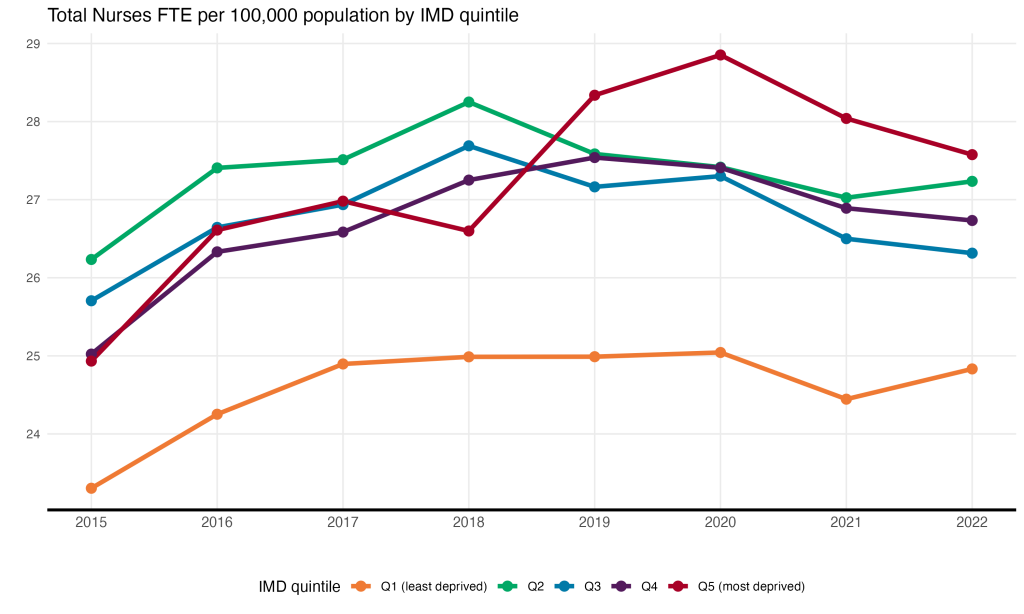
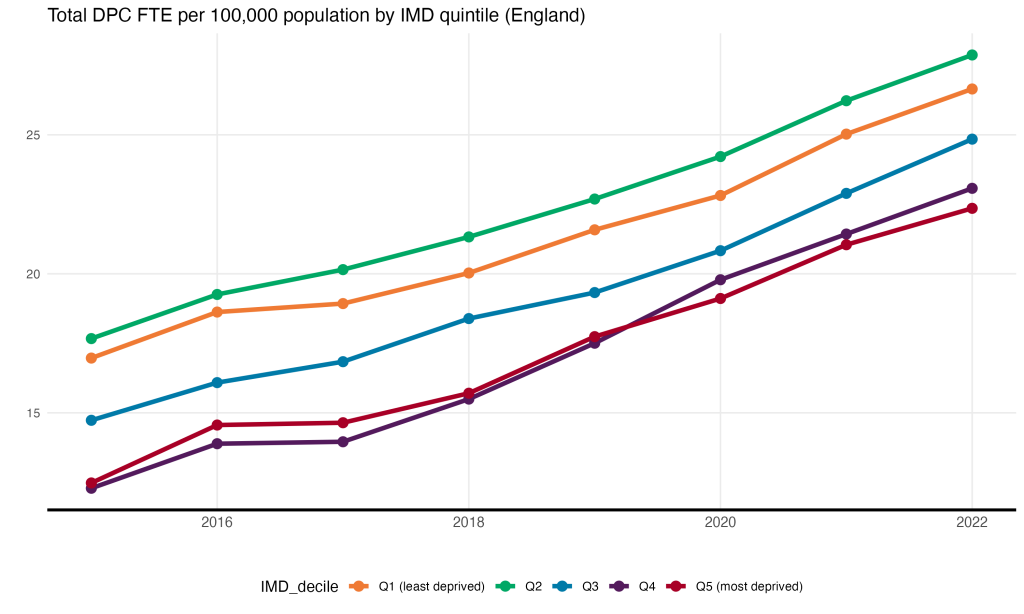
How is the workforce distributed across deprivation quintiles?
The number of staff that each practice employs is important because it impacts on the number of appointments they can offer. Funding, workforce availability, practice culture and neighbourhood factors all contribute to staffing levels within a practice. Here we have mapped the socio-economic gradient of GPs, nurses and Direct Patient Care staff (DPC, staff who treat patients but are not GPs or nurses) in each ICB.
In 2022, practices serving the most deprived 20% of the national population had 4.2 more DPC staff per 100,000 population than the practices serving the top quintile.
What is the impact of inequalities in population need, funding and workforce?
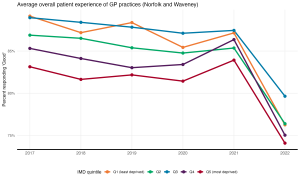
There is a mismatch in supply (funding and workforce) and demand/need (weighted population and deprivation) patterned across the socio-economic gradient. This mismatch leads to inequalities in patient experience of general practices, as measured by the GP Patient Survey.
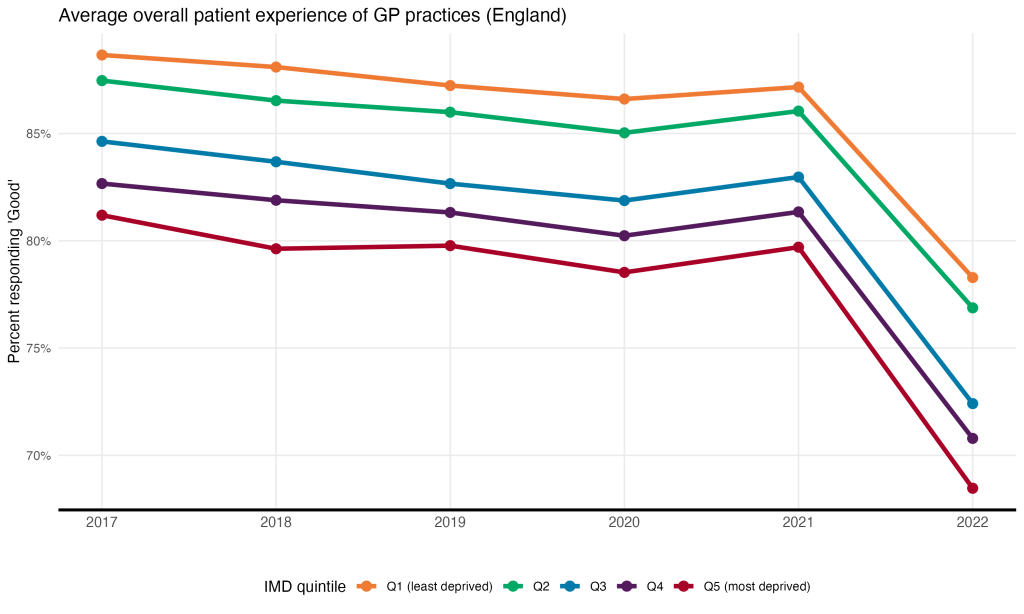
This chart shows how patient satisfaction with GP practices has changed over time by socio-economic group across England. We see that in 2015, 89% of patients who visited practices serving the least deprived quintile described their overall experience as ‘Good’, versus 81% of patients visiting practices serving the most deprived 20%. This disparity increased following a decline in patient satisfaction across the board in 2022, from 8% to 10%.
Here we explore structural determinants of inequalities at the ICB level, focussing on the East of England.
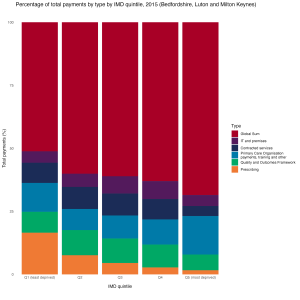
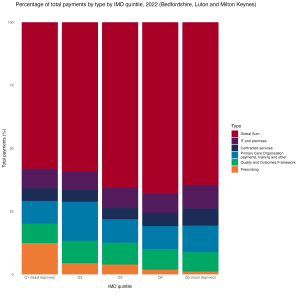
Bedfordshire, Luton and Milton Keynes
Only 2 practices in Bedfordshire, Luton and Milton Keynes, predominantly serve patients in the most deprived 20% of the national population, whereas the majority (34) of practices serve the least deprived patients.
8 years ago, practices serving the most deprived quintile (Q1) received £33 more per weighted patient than those serving the least deprived quintile. The total NHS payments per weighted patient was £138. Over the next 7 years, Q1 received steadily less per patient, while the payments to the rest of the practices increased. In 2022, the total NHS payments per weighted patient was £153, and the difference between the top and bottom quintile was -£18.
Next, we consider which category of payments caused this disparity. Payments to practices serving the most deprived quintile fell across all categories, but in percentage terms, prescribing payments and Primary Organisation payments fell the most.
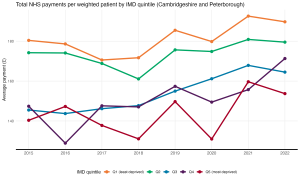
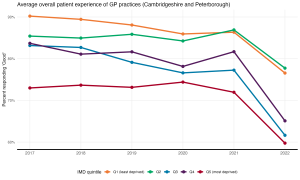
Cambridgeshire and Peterborough
In 2022, practices in Cambridgeshire and Peterborough serving the least deprived quintile received £36 more than practices serving the most deprived quintile.
16.9% fewer patients in the most deprived quintile described their overall experience as ‘Good’ than those in the least deprived quintile.
Hertfordshire and West Essex
None of the practices in Hertfordshire and West Essex serve patients who are predominantly in the most deprived 20% of the national population. A socio-economic gradient still exists, however, as the difference in average payments between practices serving the most deprived population in the ICB and the least in 2022 was £17.
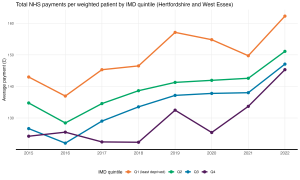
Only half (53.4%) of patients visiting practices in Q4 described their experience as ‘Good’, versus 77% of patients visiting practices in Q1.
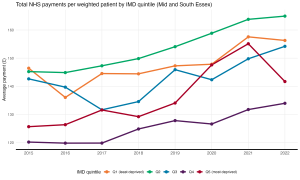
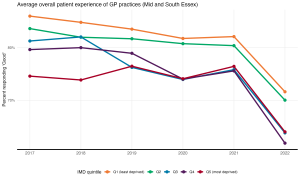
Mid and South Essex
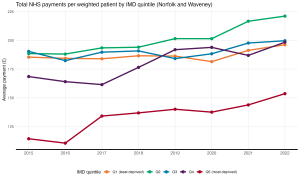
Norfolk and Waveney
Suffolk and North East Essex
Appendix
- Weighted population calculation
- Payment categories
- Global sum
- IT and premises
- Contracted services
- Primary Care Organisation payments, training and other: includes blah blah blah
- Quality and Outcomes Framework
- Prescribing
